Overcoming Insomnia: A Guide to Cognitive Behavioral Therapy for Insomnia (CBT I)
Feb 17, 2025 / zsfcdn103/
What is Cognitive Behavioral Therapy for Insomnia (CBT-I)?
Understanding Cognitive Behavioral Therapy for Insomnia (CBT-I)
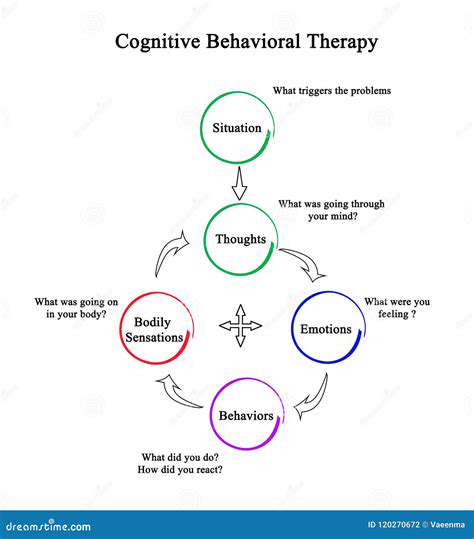
Cognitive Behavioral Therapy for Insomnia (CBT-I) is a non-pharmacological approach that aims to address the underlying cognitive and behavioral factors contributing to insomnia. This type of therapy is highly effective in treating insomnia and has been shown to produce long-term results. CBT-I is a problem-focused approach that helps individuals identify and change negative thought patterns and behaviors that contribute to their insomnia. By working with a trained therapist, individuals can learn new skills and strategies to manage stress, anxiety, and other factors that may be interfering with their sleep. Additionally, CBT-I can be tailored to meet the specific needs of each individual, making it a highly personalized and effective treatment approach. Cognitive behavioral therapy for insomnia typically involves a combination of cognitive restructuring, relaxation training, and sleep hygiene education. Overall, CBT-I is a safe and effective treatment option for individuals struggling with insomnia, and it can be used in conjunction with other therapies or as a standalone treatment.
One of the key components of CBT-I is the identification and challenge of negative thought patterns and beliefs that contribute to insomnia. This involves helping individuals become aware of their thoughts and feelings about sleep and challenging any unrealistic or unhelpful beliefs they may hold. For example, an individual may believe that they need to get eight hours of sleep each night or they will not be able to function the next day. While this may be a common belief, it is not necessarily true, and challenging this belief can help individuals develop a more realistic and positive attitude towards sleep. Furthermore, CBT-I can help individuals develop relaxation techniques, such as deep breathing, progressive muscle relaxation, and mindfulness meditation, to manage stress and anxiety that may be contributing to their insomnia. By learning these skills, individuals can better manage their stress and anxiety, leading to improved sleep quality and duration.
In addition to cognitive restructuring and relaxation training, CBT-I also involves sleep hygiene education. This includes teaching individuals about the importance of maintaining a consistent sleep schedule, creating a relaxing sleep environment, and avoiding stimulating activities before bedtime. By establishing a consistent sleep schedule and creating a relaxing sleep environment, individuals can improve the quality of their sleep and increase the likelihood of getting a full night's rest. Sleep hygiene education also involves teaching individuals about the importance of avoiding caffeine, nicotine, and electronics before bedtime, as these can all interfere with sleep. By making these changes, individuals can create an environment that is conducive to sleep and improve the overall quality of their rest. Overall, sleep hygiene education is an important component of CBT-I, and it can have a significant impact on an individual's ability to get a good night's sleep.
Cognitive behavioral therapy for insomnia can be delivered in a variety of formats, including individual therapy, group therapy, and online therapy. Each of these formats has its own advantages and disadvantages, and the best approach will depend on the individual's needs and preferences. Individual therapy, for example, provides a high level of personalized attention and support, but it can be more expensive than group therapy. Group therapy, on the other hand, provides a sense of community and support, but it may not be as effective for individuals who require a high level of personalized attention. Online therapy is a convenient and flexible option, but it may not be suitable for individuals who require a high level of interaction and support. Ultimately, the best approach will depend on the individual's needs and preferences, and a trained therapist can help determine the most effective treatment plan.
CBT-I has been shown to be highly effective in treating insomnia, and it has a number of advantages over other treatments. For example, it is a non-pharmacological approach, which means that it does not involve the use of medication. This can be beneficial for individuals who are concerned about the potential side effects of sleep medications or who have experienced negative reactions to these medications in the past. Additionally, CBT-I can be used in conjunction with other therapies, such as relaxation training or sleep hygiene education, to provide a comprehensive treatment approach. By addressing the underlying cognitive and behavioral factors contributing to insomnia, CBT-I can help individuals achieve long-term improvements in sleep quality and duration. Furthermore, CBT-I can be tailored to meet the specific needs of each individual, making it a highly personalized and effective treatment approach.
Implementing Cognitive Behavioral Therapy for Insomnia (CBT-I) in Daily Life
Implementing CBT-I in daily life requires a commitment to making changes to one's habits and behaviors. This can involve establishing a consistent sleep schedule, creating a relaxing sleep environment, and avoiding stimulating activities before bedtime. It can also involve practicing relaxation techniques, such as deep breathing or progressive muscle relaxation, to manage stress and anxiety. By making these changes, individuals can improve the quality of their sleep and increase the likelihood of getting a full night's rest. Additionally, CBT-I can involve keeping a sleep diary to track sleep patterns and identify areas for improvement. This can be a helpful tool for individuals who are trying to understand their sleep patterns and make changes to improve the quality of their rest.
One of the key challenges of implementing CBT-I in daily life is the need to make significant changes to one's routine and habits. This can be difficult, especially for individuals who are used to staying up late or engaging in stimulating activities before bedtime. However, by making these changes, individuals can improve the quality of their sleep and increase the likelihood of getting a full night's rest. It is also important to be patient and consistent when implementing CBT-I, as it can take time to see results. By working with a trained therapist and making a commitment to change, individuals can overcome insomnia and achieve improved sleep quality and duration. Furthermore, CBT-I can be tailored to meet the specific needs of each individual, making it a highly personalized and effective treatment approach.
CBT-I can also be used in conjunction with other therapies, such as relaxation training or sleep hygiene education, to provide a comprehensive treatment approach. For example, an individual may work with a therapist to develop a relaxation technique, such as deep breathing or progressive muscle relaxation, to manage stress and anxiety before bedtime. They may also receive education on sleep hygiene, such as the importance of maintaining a consistent sleep schedule and creating a relaxing sleep environment. By addressing the underlying cognitive and behavioral factors contributing to insomnia, CBT-I can help individuals achieve long-term improvements in sleep quality and duration. Additionally, CBT-I can be delivered in a variety of formats, including individual therapy, group therapy, and online therapy, making it a flexible and convenient treatment option.
In addition to its effectiveness in treating insomnia, CBT-I has a number of other benefits. For example, it can help individuals develop a more positive and realistic attitude towards sleep, which can lead to improved overall health and well-being. It can also help individuals develop coping skills and strategies to manage stress and anxiety, which can be beneficial in a variety of areas of life. Furthermore, CBT-I can be used to treat a range of sleep disorders, including insomnia, sleep apnea, and restless leg syndrome. By addressing the underlying cognitive and behavioral factors contributing to these disorders, CBT-I can help individuals achieve improved sleep quality and duration, leading to improved overall health and well-being.
Overall, CBT-I is a highly effective treatment approach for insomnia, and it has a number of advantages over other treatments. By addressing the underlying cognitive and behavioral factors contributing to insomnia, CBT-I can help individuals achieve long-term improvements in sleep quality and duration. It is a non-pharmacological approach, which means that it does not involve the use of medication, and it can be tailored to meet the specific needs of each individual. Additionally, CBT-I can be used in conjunction with other therapies, such as relaxation training or sleep hygiene education, to provide a comprehensive treatment approach. By working with a trained therapist and making a commitment to change, individuals can overcome insomnia and achieve improved sleep quality and duration, leading to improved overall health and well-being.
Key Components of CBT-I:
Understanding Sleep Hygiene
Sleep hygiene is a foundational element of CBT-I, representing a collection of habits and practices designed to promote sound sleep. This involves establishing a consistent sleep schedule, which means going to bed and waking up at the same time every day, even on weekends, to regulate your body's natural sleep-wake cycle, also known as your circadian rhythm. Furthermore, the sleep environment plays a critical role; your bedroom should be dark, quiet, and cool, creating a relaxing and conducive atmosphere for sleep, minimizing disruptions from external factors like light, noise, and excessive temperatures, which can significantly impact your sleep quality and make it harder to fall asleep.
Another pivotal aspect of sleep hygiene is the avoidance of stimulating substances and activities before bed. This encompasses limiting caffeine and alcohol consumption, especially in the hours leading up to sleep, as these substances can interfere with your ability to fall asleep and stay asleep throughout the night. Similarly, it also involves refraining from engaging in stimulating activities like watching television or using electronic devices, which emit blue light that can suppress melatonin production and disrupt your sleep cycle, further impacting your ability to obtain proper restorative sleep and wake up feeling refreshed.
Stimulus Control Therapy
Stimulus control therapy is a technique designed to strengthen the association between your bed and sleep, weakening the connection between the bed and wakefulness or activities that are not sleep-related. The core principle involves establishing strict rules about when you should be in bed and what you should be doing there. Only go to bed when you are sleepy, avoiding activities like reading, watching television, or working in bed, to prevent associating your bed with wakefulness and other stimulating non-sleep activities, which would make it increasingly difficult to fall asleep.
If you are unable to fall asleep within a certain timeframe, typically 20 minutes, the stimulus control therapy suggests that you get out of bed and go to another room to engage in a relaxing activity until you feel sleepy. Then, you should return to bed only when you feel drowsy, repeating this process as many times as necessary throughout the night. This procedure helps to re-establish the bed as a cue for sleep, which then strengthens your circadian rhythm, and minimizes the anxiety and frustration often associated with lying awake in bed, which can contribute to a cycle of poor sleep.
Sleep Restriction Therapy
Sleep restriction therapy aims to consolidate your sleep by limiting the amount of time you spend in bed, aligning the time spent in bed more closely with the actual time you spend sleeping. This approach may seem counterintuitive, as it restricts the time spent in bed; however, the intention is to increase your sleep drive, making you feel more tired and ready to sleep during the designated sleep period. Initially, your time in bed is restricted, and the goal is to gradually increase this time as your sleep efficiency, which measures the amount of time you are actually sleeping when in bed, improves.
A sleep diary is frequently used to determine your current sleep patterns and calculate the appropriate amount of time to spend in bed. By consistently tracking the time you go to bed, the time you wake up, and the number of times you wake up during the night, you can obtain valuable data needed to identify patterns and determine your sleep efficiency, and tailor sleep restriction plans. The sleep restriction plan is then adjusted periodically to ensure that the time in bed is optimized and the process will help increase the intensity of your sleep drive, leading to better sleep, more efficiently, and reducing the time you spend in bed awake and restless, which reduces anxiety around the subject.
Cognitive Therapy for Insomnia
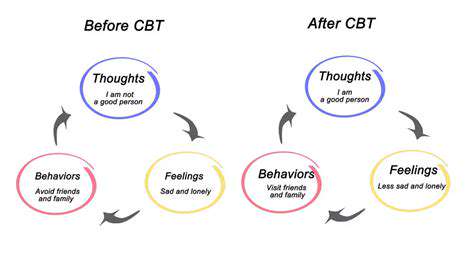
Cognitive therapy for insomnia focuses on identifying and challenging negative thoughts and beliefs about sleep that contribute to insomnia. These cognitions can include catastrophic thinking about the consequences of not sleeping, such as exaggerated worries about daytime functioning, performance, or health issues, which lead to anxiety and increased alertness, making it more difficult to fall asleep. It also involves the identification of maladaptive beliefs about sleep, such as the need for a specific amount of sleep, or the fear of not sleeping enough, and this fear perpetuates a cycle of anxiety and insomnia, making sleep more challenging.
Techniques like cognitive restructuring are used to replace these negative thoughts with more realistic and balanced perspectives. This approach encourages you to critically evaluate your thoughts and feelings, recognizing distortions, and reframing them in a way that reduces anxiety and promotes a more positive outlook on sleep. For example, you can actively challenge the thought, “I need eight hours of sleep to function properly,” by providing a more rational thought, such as, “I may need less sleep, and I will be okay.” This method will help you recognize and change your sleep-related beliefs and develop more adaptive coping strategies that ultimately improve sleep quality and reduce the impact of insomnia on your daily life by creating more adaptive cognitive strategies.
Is CBT-I Right for You?
Understanding the Core Principles of CBT-I
Cognitive Behavioral Therapy for Insomnia (CBT-I) is a structured program meticulously designed to identify and change the thoughts and behaviors that contribute to sleep problems. It operates on the fundamental principle that insomnia is often perpetuated by a cycle of negative thoughts and learned behaviors. CBT-I, in its essence, addresses the underlying causes of sleep disturbance rather than merely masking the symptoms, thereby offering a more sustainable and long-lasting solution to chronic insomnia sufferers, enabling a more profound and comprehensive improvement in sleep quality overall.
One of the primary focuses of CBT-I is cognitive restructuring, which involves recognizing and challenging the negative thoughts and beliefs individuals harbor about sleep, such as the catastrophic anticipation of sleepless nights. These distorted thoughts, like the fear of not sleeping well, often amplify anxiety and create a self-fulfilling prophecy, which severely impacts sleep and generates emotional distress. Addressing these maladaptive thought patterns helps individuals reduce the anxiety that fuels insomnia and develop a more realistic and less fearful approach to sleep, ensuring a more relaxed state conducive to rest and rejuvenation.
Behavioral techniques within CBT-I also play a pivotal role, targeting habits and routines that interfere with sleep, including irregular sleep schedules or spending excessive time in bed. These behavioral modifications encompass techniques like sleep restriction, stimulus control, and relaxation exercises. Sleep restriction, for instance, strategically limits the time spent in bed to match actual sleep duration, creating a mild sleep deprivation to increase sleep drive, ultimately improving sleep efficiency and consolidation, while stimulus control helps to re-associate the bed with sleep instead of activities that may interfere with sleep. These approaches, when implemented effectively, promote a more regular and restful sleep cycle.
Furthermore, the principles of CBT-I extend beyond addressing immediate sleep challenges and often incorporate psychoeducation to increase the patient’s understanding of sleep, insomnia, and the treatment itself. This is a crucial aspect of CBT-I as patients' active participation through self-monitoring of sleep patterns is crucial. Through education, individuals gain a deeper understanding of the biological and psychological factors that impact sleep, as well as a comprehensive ability to self-manage and maintain the skills learned throughout the CBT-I treatment to achieve optimal sleep hygiene throughout their lives, ensuring consistent long-term benefits.
Overall, the multi-faceted approach of CBT-I which combines cognitive and behavioral strategies helps patients break the cycle of insomnia by addressing both the thoughts and behaviors that contribute to sleep problems. This holistic approach, when carefully tailored to an individual's needs, ultimately allows the individual to regain control over their sleep, and experience a sustained improvement in sleep quality and overall well-being. The therapy is not just about fixing the problem in the short term but also about equipping individuals with the necessary tools and knowledge to manage their sleep long term and achieve a better quality of life.
The Common Techniques Used in CBT-I
Stimulus control is a cornerstone technique within Cognitive Behavioral Therapy for Insomnia, designed to re-associate the bedroom and bed specifically with sleep, and to reduce the association with wakefulness, anxiety, and other activities. This method helps to break the connection between the bed and things like tossing and turning, watching television, or browsing on a smartphone, which could ultimately hinder the sleep process. The goal is to reinforce the bedroom as a cue for sleep; this often involves strict rules such as only going to bed when sleepy and getting out of bed if unable to fall asleep within a reasonable time (usually 20 minutes) and only returning when feeling tired again, ensuring the bedroom is viewed as a space solely for sleep.
Sleep restriction, another integral component of CBT-I, involves carefully limiting the time spent in bed to match the actual time spent sleeping, resulting in a mild state of sleep deprivation, which dramatically enhances the drive to sleep and improves sleep efficiency. By restricting the time in bed, the body’s natural sleep drive intensifies, therefore, individuals can fall asleep quicker and experience fewer awakenings during the night. Over time, and as sleep improves, the time spent in bed is gradually increased, which allows the patient to restore a more natural sleep schedule, while also minimizing the potential for daytime sleepiness, ensuring a balanced approach to managing insomnia and promoting better health.
Cognitive restructuring focuses on identifying and changing the unhelpful thoughts and beliefs about sleep that can perpetuate insomnia. Common examples include catastrophizing about the consequences of a bad night's sleep, overestimating the impact of sleep loss, or holding unrealistic expectations about the amount of sleep required. This component of CBT-I equips individuals with cognitive tools to help them challenge and modify such thoughts. The main objective of cognitive restructuring helps patients develop more realistic and balanced perspectives on sleep, thereby reducing anxiety and improving the likelihood of falling asleep and staying asleep, and eventually, helping them overcome their fears of insomnia.
Relaxation techniques are often integrated into CBT-I to reduce physiological and psychological arousal that can interfere with sleep onset and maintenance. This might involve progressive muscle relaxation, deep breathing exercises, meditation, or guided imagery to calm the body and mind before bed. Regular use of these techniques can lead to improved sleep quality, reduced stress levels, and an overall sense of well-being, promoting an environment where sleep becomes easier and more restorative. When integrated, these techniques help patients to develop a routine conducive to a calm state, increasing the chances of restful sleep, and promoting a healthier relationship with sleep.
Finally, sleep hygiene education forms an essential part of CBT-I, providing individuals with crucial information about healthy sleep habits. It incorporates guidance on creating a conducive sleep environment, establishing a regular sleep-wake schedule, avoiding caffeine and alcohol before bed, and incorporating regular exercise into the day. Through this knowledge, individuals become empowered to make lifestyle changes that support better sleep. Following these sleep hygiene guidelines provides the foundation for lasting sleep improvements, as patients proactively manage their sleep through their daily behaviors and routines.
Determining If CBT-I is the Right Approach for You
Evaluating the suitability of CBT-I requires careful consideration of several factors, including the type and severity of your insomnia symptoms, any co-occurring medical or psychiatric conditions, and your personal preferences and willingness to engage in the therapeutic process. Firstly, understanding the characteristics of your insomnia is crucial, as CBT-I is most effective for primary insomnia, where sleep difficulties are not directly caused by another underlying medical or psychological condition, providing the most significant relief. It is important to distinguish between acute, transient insomnia and chronic insomnia. Chronic insomnia, characterized by persistent sleep problems for at least three months, often benefits more from the structured approach that CBT-I provides, offering a more targeted treatment plan.
Secondly, individuals with co-existing mental health conditions such as depression, anxiety, or PTSD might benefit from CBT-I, but it is essential to consider how these conditions may impact treatment and may need to be addressed concurrently. For example, individuals experiencing significant depression or anxiety might require additional therapeutic interventions or medication management alongside CBT-I, ensuring all factors are treated in a coordinated fashion. Discussing these conditions with your doctor can help determine if CBT-I will meet all of your needs, and also help develop a comprehensive treatment plan, improving the overall effectiveness of the process and improving the overall effectiveness of treatment.
Thirdly, it is crucial to consider your motivation and commitment to the CBT-I process. CBT-I is not a passive treatment, but instead requires active participation, including the adherence to prescribed behavioral changes, the completion of sleep diaries, and the cognitive challenging of negative thoughts. Success in CBT-I depends on the individual’s willingness to make adjustments to their lifestyle and thought patterns. Patients need to be prepared to invest time and effort into the program to fully realize its benefits and develop the skills and knowledge to improve sleep quality and duration. Therefore, patient compliance and a proactive approach are critical determinants of successful CBT-I treatment.
Additionally, consider your access to qualified CBT-I providers, such as clinical psychologists, psychiatrists, or other mental health professionals with specialized training in CBT-I. The availability of these professionals may vary depending on your location and insurance coverage. Also, the length and format of the sessions can vary, but typically CBT-I includes a series of weekly or bi-weekly sessions over several weeks. Finding a therapist with whom you feel comfortable and supported is crucial, as the therapeutic relationship plays an essential role in the effectiveness of the therapy. In addition to this, understanding the format, including in-person, online, or group settings, can help determine the best option for the individual’s needs and circumstances, ensuring convenience, accessibility, and overall satisfaction.
Finally, it is important to consult with a healthcare professional, such as your primary care physician or a sleep specialist, to determine if CBT-I is an appropriate and safe treatment option for your specific situation. This consultation should involve a thorough evaluation of your sleep history, medical history, and current medication regimen to rule out any underlying medical conditions that may be contributing to your sleep problems. They can discuss the potential benefits and risks of CBT-I, provide referrals to qualified providers, and help you determine the most appropriate course of action to manage your insomnia and to improve your overall health and well-being, offering you the best possible care for your unique needs and to improve your overall quality of life.