Narcolepsy: Symptoms, Causes, and Management Techniques
Nov 21, 2024 / zsfcdn103/
Common Symptoms of Narcolepsy
Excessive Daytime Sleepiness
One of the hallmark symptoms of narcolepsy is excessive daytime sleepiness (EDS). This condition can make individuals feel uncontrollably sleepy during the day, regardless of how much sleep they got the night before. People often report finding it difficult to stay awake in situations such as meetings or while watching television.
The sleepiness experienced can vary in intensity, with some individuals feeling only mildly drowsy, while others may experience sudden sleep attacks. These can occur without warning and may last from a few seconds to several minutes. Such unpredictability can impact daily activities, making it difficult to perform work or maintain social relationships.
EDS may lead individuals to nap frequently throughout the day, but these naps often do not provide the restorative benefits that many expect. Instead, these naps might exacerbate the overall condition, leading to a cycle of fatigue. Understanding the importance of managing this symptom is crucial for those diagnosed with narcolepsy.
Psychological and emotional factors, such as stress and anxiety, can intensify excessive daytime sleepiness. People sometimes experience cognitive impairments, such as problems with memory and concentration, further complicating their ability to function effectively.
Addressing EDS often involves a combination of medication, lifestyle changes, and behavioral strategies. Patients should work closely with their healthcare providers to develop a comprehensive management plan tailored to their specific needs.
Cataplexy and Its Impact
Cataplexy is another significant symptom associated with narcolepsy and is characterized by sudden muscle weakness or loss of muscle tone, often triggered by strong emotions such as laughter, anger, or surprise. This phenomenon can be startling for both the person experiencing it and those around them.
During a cataplectic episode, an individual may experience a range of muscle control issues, from slurred speech to complete collapse. The duration of these episodes typically varies; they can last from a few seconds to a couple of minutes, and while consciousness remains intact, the inability to move can be distressing.
Cataplexy can severely impact a person's quality of life, leading to avoidance of social situations or activities that provoke strong emotions. Many individuals with narcolepsy report feeling isolated due to the unpredictability of these attacks, which can lead to anxiety and depression.
Management strategies for cataplexy often include lifestyle modifications, such as learning to recognize triggers and adopting coping mechanisms. Medications can also play a crucial role in reducing the frequency and severity of episodes, helping individuals regain a sense of control over their lives.
Understanding and addressing cataplexy is essential for individuals and their families, promoting awareness and reducing stigma. Education and support from healthcare professionals can empower individuals to manage this challenging symptom effectively.
Sleep Disruptions and Nighttime Symptoms
Patients with narcolepsy often experience significant disruptions in their nighttime sleep patterns. Despite feeling excessively sleepy during the day, many struggle with maintaining a consistent and restful full night's sleep. Frequent awakenings throughout the night can lead to increased fatigue and confusion during the waking hours.
Common nighttime symptoms include insomnia, rapid eye movement (REM) sleep behavior disorder, and sleep paralysis. Insomnia can manifest as difficulty falling asleep, staying asleep, or waking too early. Sleep paralysis, on the other hand, occurs when a person is temporarily unable to move or speak, often while falling asleep or waking up, which can be a frightening experience.
Additionally, hypnagogic hallucinations may occur, characterized by vivid and often frightening preludes to falling asleep or waking. This can exacerbate feelings of anxiety and fatigue, creating a challenging cycle for those affected.
To manage these nighttime symptoms, individuals can benefit from establishing a consistent sleep schedule and creating a calming bedtime routine. Cognitive behavioral therapy (CBT) can also be helpful for addressing sleep issues and anxiety related to sleep disturbances.
Collaboration with healthcare providers is essential for developing an effective approach to managing nighttime symptoms. By combining lifestyle changes, therapeutic interventions, and, if appropriate, medication, patients can work towards achieving better sleep quality and an improved overall quality of life.
Causes of Narcolepsy

Genetic Factors
Narcolepsy has been observed to have a genetic component, with certain genes linked to an increased risk of developing the condition. Research shows that individuals with family histories of narcolepsy are more likely to experience symptoms themselves.
One of the key genetic markers identified is the HLA-DQB1*06:02 allele, which is present in a significant percentage of those diagnosed. However, not everyone with this genetic marker will develop narcolepsy, indicating that other factors also play a role.
Environmental Triggers
Environmental factors can trigger the onset of narcolepsy in individuals who are genetically predisposed. Factors such as viral infections, especially those affecting the central nervous system, have been associated with the onset of this disorder.
Various studies have suggested that infections, particularly during childhood, may accelerate the development of narcoleptic symptoms in genetically susceptible individuals. This highlights the complex interplay between genetics and environmental influences.
Neurological Changes
The pathophysiology of narcolepsy involves significant neurological changes, especially in the hypothalamus, which plays a crucial role in regulating sleep. In patients with narcolepsy, there is often a reduction of hypocretin (orexin) neurons, which are vital for maintaining wakefulness.
The loss of these neurons can lead to disrupted sleep-wake cycles, resulting in excessive daytime sleepiness and other characteristic symptoms of narcolepsy. Understanding these neurological changes is essential for developing targeted treatments and management strategies.
Autoimmune Responses
Some researchers hypothesize that narcolepsy may be an autoimmune disorder, where the body's immune system mistakenly attacks the hypocretin-producing neurons. This perspective is strengthening as more cases of narcolepsy coincide with autoimmune diseases and responses.
Identifying narcolepsy as an autoimmune condition could reshape our approach to treatment, focusing on modulating immune responses to prevent further loss of hypocretin neurons. Such insights into the underlying causes of narcolepsy can pave the way for innovative therapeutic options.
Management Techniques for Narcolepsy
Behavioral and Lifestyle Modifications
One significant aspect of managing narcolepsy involves making lifestyle changes that promote better sleep hygiene. This includes establishing a consistent sleep schedule, going to bed and waking up at the same time every day, even on weekends. Maintaining a routine helps regulate the body’s internal clock, which can mitigate some of the symptoms associated with narcolepsy.
In addition to a sleep schedule, incorporating short naps into the day can be incredibly beneficial for individuals with narcolepsy. Napping for 10 to 20 minutes can help alleviate excessive daytime sleepiness and improve overall alertness. However, it is essential to limit the duration of these naps to prevent grogginess and disruption of nighttime sleep.
Moreover, creating a restful sleep environment by minimizing noise, light, and other distractions can enhance sleep quality. Simple techniques such as using blackout curtains, white noise machines, and keeping the bedroom at a comfortable temperature can make a significant difference in managing narcolepsy symptoms.
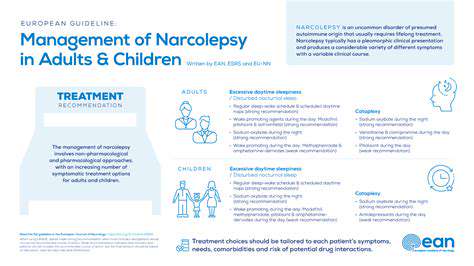
Medical and Therapeutic Interventions
Various medical treatments are available for managing narcolepsy symptoms, primarily focusing on improving wakefulness and reducing episodes of cataplexy. Stimulant medications, such as modafinil, are often prescribed to help combat excessive daytime sleepiness. Additionally, sodium oxybate has been shown to effectively reduce nighttime symptoms and improve overall alertness during the day.
Alongside medication, cognitive behavioral therapy (CBT) can be an effective approach for some individuals. CBT focuses on reshaping negative thought patterns related to sleep and developing coping strategies to manage symptoms more effectively. This therapeutic intervention helps narcolepsy patients gain better control over their condition and supports overall mental health.
Collaboration with healthcare professionals is crucial in creating a tailored management plan for narcolepsy. Regular follow-ups with doctors and sleep specialists can help optimize treatment effectiveness and make necessary adjustments, ensuring that individuals lead a more fulfilling and active life.