Cognitive Behavioral Therapy for Insomnia: How It Works
Mar 03, 2025 / zsfcdn103/
Outline
Insomnia disrupts life, causing fatigue and decreased cognitive function.
CBT-I improves sleep by changing negative thought patterns.
CBT-I is effective without the side effects of medications.
Sleep diaries help track patterns and improve strategies for sleep.
Relaxation techniques reduce anxiety associated with insomnia.
Improved sleep from CBT-I leads to better mental health outcomes.
Structured steps in CBT-I address habits causing insomnia.
Consistency in sleep hygiene fosters a conducive sleep environment.
Stimulus control reinforces sleep association with the bed.
Managing anxiety and stress is crucial in combating insomnia.
Sleep restriction aligns actual sleep times with bed hours.
Lifestyle adjustments enhance long-term sleep quality significantly.
CBT-I fosters self-management and confidence in sleep health.
Clients report lasting improvements in sleep even post-therapy.
What is Cognitive Behavioral Therapy for Insomnia (CBT-I)?
Understanding Insomnia and Its Effects
Insomnia is a prevalent sleep disorder characterized by difficulty falling or staying asleep. This condition can severely affect an individual’s quality of life, leading to fatigue, irritability, and decreased cognitive function during waking hours. People suffering from insomnia may find themselves in a perpetual cycle of sleep deprivation that exacerbates their overall mental health.
It can manifest in various forms, including acute insomnia, which lasts for a short duration, and chronic insomnia, persisting for months or years. The causes of insomnia can be multifactorial, incorporating stress, anxiety, medical conditions, and lifestyle choices that disrupt normal sleep patterns. Understanding these underlying factors is crucial for effective treatment and management.
The impact of insomnia extends beyond merely being unable to sleep; it can contribute to more serious health conditions such as cardiovascular diseases, diabetes, and depression. Over time, the physical toll becomes apparent, significantly reducing one's overall well-being and productivity. Awareness of these potential consequences serves as a powerful motivator for seeking appropriate treatment.
Additionally, insomnia often creates a negative feedback loop. Poor sleep leads to daytime dysfunction, which can increase anxiety and stress, thereby perpetuating the sleep problem. Recognizing this cycle is critical in addressing the issue comprehensively, paving the way for strategies such as Cognitive Behavioral Therapy for Insomnia.
Understanding insomnia's various dimensions encourages individuals to pursue effective treatment options. Seeking professional help for insomnia not only aims to alleviate the immediate symptoms but also addresses the deeper issues contributing to this challenging condition.
The Principles of Cognitive Behavioral Therapy for Insomnia
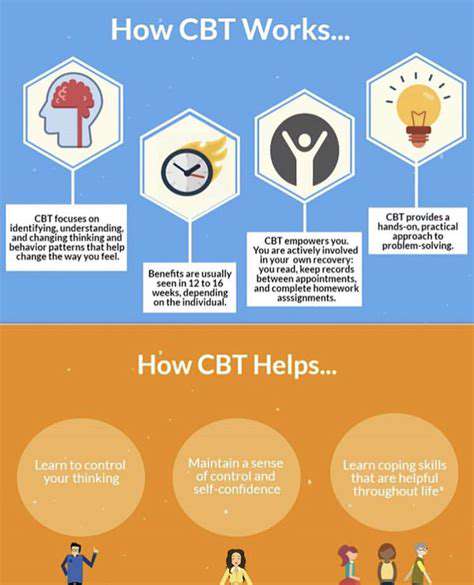
Cognitive Behavioral Therapy for Insomnia (CBT-I) operates on the premise that changing negative thought patterns can improve sleep. Unlike traditional sleep medications, CBT-I targets the cognitive and behavioral patterns that contribute to insomnia. The therapy encompasses practices that encourage healthier sleep habits and attitudes towards sleep.
CBT-I generally takes place over several sessions with a trained therapist, focusing on understanding thoughts related to sleep and devising personalized strategies. The therapy process includes education, techniques for sleep restriction, and cognitive restructuring to challenge dysfunctional beliefs about sleep.
A core aspect of CBT-I is the sleep diary, which helps clients track their sleep patterns and identify behaviors that may be contributing to insomnia. Through consistent monitoring, individuals can glean insights into their sleep habits, leading to more focused changes in their nightly routines.
Additionally, CBT-I equips individuals with relaxation techniques to alleviate anxiety associated with sleep. Methods such as progressive muscle relaxation and mindfulness meditation are often integrated, helping to lower physiological arousal and create a more conducive environment for rest.
Overall, the structured approach of CBT-I not only addresses the symptoms of insomnia but also helps to instill long-lasting changes in behavior and thought processes about sleep, ultimately leading to better sleep quality over time.
Benefits of CBT-I Compared to Traditional Treatments
Cognitive Behavioral Therapy for Insomnia shows numerous advantages over conventional treatments, such as sleep medications. Unlike medications, which often come with potential side effects and dependency issues, CBT-I promotes sustainable, long-term solutions for sleep problems. Clients learn self-regulating strategies that empower them to manage their insomnia without reliance on pharmacological interventions.
Moreover, CBT-I addresses the root causes of insomnia rather than merely masking the symptoms. This holistic approach allows individuals to develop healthier sleep patterns and coping mechanisms, which facilitates greater resilience against future sleep issues. Over time, users often report improved well-being and sleep satisfaction.
Research has demonstrated that CBT-I is highly effective, with many studies noting that participants experience significant improvements in sleep quality and overall functioning. This efficacy often lasts well beyond the completion of therapy, showcasing the long-term benefits of CBT-I.
CBT-I is also accessible and adaptable. Many therapists now offer online sessions, making it easier for individuals to engage in treatment regardless of geographical constraints. This accessibility ensures that more people can benefit from the science-backed techniques offered through CBT-I.
Ultimately, the effectiveness, sustainability, and accessibility of CBT-I make it a compelling option for anyone struggling with insomnia. It not only aids in achieving immediate relief from sleep troubles but also encourages a healthier relationship with sleep over the long term.
Steps Involved in Cognitive Behavioral Therapy for Insomnia
The process of engaging in Cognitive Behavioral Therapy for Insomnia typically unfolds through several structured steps. Initially, an assessment helps the therapist and client understand the severity of the sleep issues and explore specific behaviors and thoughts contributing to the insomnia. This cooperative approach establishes a foundation for the entire therapeutic journey.
Next, clients are often introduced to sleep hygiene practices, which include recommendations for creating a sleep-friendly environment and establishing a consistent sleep schedule. By promoting these foundational habits, individuals can immediately enhance their chances of restful sleep.
As therapy progresses, cognitive restructuring follows, wherein clients learn to identify irrational or negative thoughts surrounding sleep—like "I can never sleep well"—and work towards replacing those thoughts with more rational beliefs. This shift in perspective is vital, as it can alleviate the pressure associated with falling asleep.
Another significant component is the practice of sleep restriction, where clients learn to limit the time spent in bed to match their actual sleep duration. This technique helps consolidate sleep and reduces the time spent awake in bed, clarifying the association between bed and sleep, instead of being a source of anxiety.
Finally, relaxation techniques such as deep breathing, visualization, or mindfulness-based practices are introduced. These techniques help to reduce the hyperarousal state often associated with insomnia, making it easier for clients to transition into a restful state at night. Through these various steps, CBT-I creates a comprehensive strategy tailored to each individual's experiences with insomnia.
Impact of CBT-I on Long-Term Sleep Quality
Cognitive Behavioral Therapy for Insomnia has proven effective not just for immediate improvements in sleep, but for fostering long-lasting changes in sleep quality. Research indicates that individuals who complete CBT-I often see sustained benefits, enjoying regular sleep patterns and experiences long after the therapy has concluded.
The principles learned during CBT-I allow clients to build a foundation for a healthier relationship with sleep. As they internalize the techniques and strategies relevant to managing their sleep, they become better equipped to face any future sleep challenges. This empowerment leads to increased confidence and reassurance that they can manage their sleep health.
In addition to improving sleep quality, CBT-I can also enhance overall mental health. Many clients report reductions in anxiety and depressive symptoms after undergoing CBT-I, attributing these ameliorations to the newfound sleep habits and coping mechanisms they've developed. Sleep is intricately connected to mental health, and better sleep can lead to enhanced well-being.
Furthermore, as individuals experience better sleep, they often witness improvements in daily functioning. Increased alertness and improved concentration during waking hours can contribute to enhanced productivity, better relationships, and a more enriched life experience. These cascading benefits highlight the powerful role of sleep in overall health.
The influence of CBT-I extends beyond just sleep. By learning and applying the techniques from this evidence-based therapy, individuals acquire skills that promote sustainable change in their lives, paving the way for a healthier and happier future—ultimately leading to a profound transformation in how they experience both sleep and life itself.
How CBT-I Works
Understanding Cognitive Behavioral Therapy for Insomnia
Cognitive Behavioral Therapy for Insomnia (CBT-I) is a structured program that helps individuals address the underlying thoughts and behaviors contributing to insomnia. It isn't just about sleep; rather, it's a comprehensive approach to fostering better sleep habits and addressing any negative beliefs surrounding sleep. This modality empowers individuals to confront and modify their disruptive sleep patterns through cognitive and behavioral strategies.
The first step in CBT-I often involves a thorough assessment of the patient's sleep habits and history. By gathering data on sleep patterns, the therapist identifies specific issues contributing to insomnia. This diagnostic phase is essential because it tailors the therapy to meet the unique needs of the individual, paving the way for effective intervention.
Throughout CBT-I, participants are educated about the sleep process and the factors that can affect it. This educational component is critical, as it allows individuals to recognize misconceptions about sleep that may lead to anxiety or stress. By demystifying sleep and explaining its biological functions, CBT-I helps reduce the fear associated with insomnia.
Cognitive restructuring is another fundamental aspect of CBT-I, where clients learn to challenge and change unhelpful thoughts about their sleep. Thoughts such as "I’ll never get to sleep" or "I need to sleep eight hours every night" can exacerbate anxiety and make sleep harder to attain. This part of therapy is vital for dismantling irrational beliefs, enabling a healthier mindset toward sleep.
Behavioral Strategies in CBT-I
Behavioral techniques included in CBT-I focus on modifying sleep habits and environments that may be detrimental to rest. One of the most powerful tools is stimulus control, which helps reinforce the connection between the bedroom and sleep. This involves creating an environment conducive to sleep by maintaining specific behaviors, such as going to bed only when feeling sleepy and getting up at the same time every day.
Another effective strategy is sleep restriction therapy, which limits the amount of time spent in bed, aiming to create a stronger association between being in bed and actually sleeping. While it may feel counterintuitive, by reducing the time spent awake in bed, individuals can cultivate a more consistent sleep pattern over time. This process of gradually increasing sleep time can lead to improved sleep efficiency and quality.
Relaxation techniques are also integral parts of CBT-I, helping to reduce the physical and mental tension that can inhibit sleep. Methods like deep breathing, progressive muscle relaxation, and mindfulness can create a state of calm that is conducive to falling asleep. These relaxation strategies can be practiced as part of a pre-sleep routine, contributing to a decline in sleep anxiety.
Finally, CBT-I emphasizes the importance of general sleep hygiene practices, which include guidelines for maintaining a sleep-friendly environment. These practices may involve use of blackout curtains, reducing screen time before bed, and creating a comfortable sleeping environment. When combined with cognitive and behavioral strategies, these hygiene practices serve to fully equip individuals with the tools they need to overcome insomnia.
1. Sleep Education
Understanding the Importance of Sleep Hygiene
Sleep hygiene refers to practices that can help improve the quality and duration of sleep. This includes maintaining a consistent sleep schedule, creating an optimal sleep environment, and being mindful of pre-sleep activities. Proper sleep hygiene is foundational to cognitive behavioral therapy for insomnia (CBT-I), as it not only facilitates sleep but also helps individuals understand and adjust their own behaviors and attitudes toward sleep.
As part of an educational initiative, it's crucial to educate individuals on factors such as the impact of light exposure on circadian rhythms, the importance of a comfortable mattress and bedding, and the role of diet and exercise in promoting restful nights. When armed with this knowledge, individuals are in a better position to implement effective changes in their routine, thereby enhancing their overall sleep quality.
The Role of Cognitive Behavioral Techniques in Sleep Education
Cognitive behavioral techniques are central to sleep education within the framework of CBT-I. These techniques aim to identify and change negative thought patterns that contribute to sleep disturbances. Individuals learn to recognize irrational beliefs about sleep, such as the notion that one must achieve a perfect eight hours to feel rested, which can lead to anxiety and further insomnia. By addressing these cognitive distortions, patients can approach sleep with a healthier mindset.
Moreover, behavioral strategies like stimulus control therapy and sleep restriction are introduced as part of the educational process. These methods help individuals develop a better association with their sleep environment, promoting stronger cues for sleep and wakefulness. Through understanding and practicing these techniques, individuals not only enhance their knowledge about effective sleep practices but also empower themselves to combat insomnia more effectively.
2. Cognitive Restructuring
Cognitive Restructuring: Understanding the Process
The process of cognitive restructuring involves identifying and challenging negative thought patterns that contribute to insomnia. This cognitive-behavioral technique is fundamental in assisting individuals to reframe their thoughts about sleep. By recognizing the cognitive distortions that lead to anxiety, individuals can learn to replace these thoughts with more productive, rational ones that promote a healthier attitude toward sleep.
During cognitive restructuring, practitioners guide clients through various techniques designed to foster self-awareness. This heightened awareness enables individuals to pinpoint irrational beliefs about sleep quality, duration, or necessity. By doing so, clients may confront fears surrounding sleeplessness and its implications, leading to reduced stress and anxiety related to falling asleep.
An essential aspect of cognitive restructuring is the practice of thought monitoring. Clients are encouraged to keep a sleep diary to track when negative thoughts arise and how they affect sleep patterns. Over time, this technique not only aids in developing insight into cognitive patterns but also illustrates the connection between thoughts and emotional responses, ultimately leading to more constructive thought habits.
Furthermore, cognitive restructuring incorporates techniques such as cognitive reframing, where individuals learn to view their sleep challenges from a different perspective. Instead of seeing insomnia as a failed attempt at rest, it can be reframed as an opportunity for personal growth and learning how to manage stress. This shift in mindset can significantly mitigate anxiety surrounding sleep.
Overall, cognitive restructuring forms a pivotal part of cognitive-behavioral therapy for insomnia, aiming to transform maladaptive thought processes into healthier beliefs, thus enhancing the quality of sleep and overall mental well-being.
Key Techniques in Cognitive Restructuring
In the realm of cognitive restructuring, several techniques can be effectively employed to assist clients in overcoming insomnia. One prominent technique is the use of Socratic questioning, which encourages individuals to critically examine their thoughts. By crafting open-ended questions, therapists facilitate a dialogue that helps clients uncover the validity of their beliefs about sleep. This exploration often helps in dispelling myths that contribute to insomnia.
Another valuable technique is cognitive behavioral exposure, where individuals gradually confront their fears about not sleeping or experiencing sleep disturbances. This approach helps to desensitize them to the anxiety associated with these thoughts and experiences, enabling a more relaxed response to sleep-related challenges. Over time, this exposure leads to reduced fear and an improvement in the overall approach towards sleep.
In addition, visualization techniques can play a significant role in cognitive restructuring. Clients may be guided to visualize a peaceful sleeping environment or a successful night of restful sleep. This mental imagery helps anchor positive thoughts and feelings associated with sleep, counteracting the negative cognition that often arises. Such practices can create a subconscious expectation of restfulness.
Behavioral activation is another method integrated into cognitive restructuring. This involves encouraging individuals to engage in positive activities during the day that can enhance mood and reduce anxiety. As mood improves, so does the body’s physiological readiness for sleep, fostering a more natural sleep cycle. Clients are encouraged to find a balance between activity and rest, which further supports healthy sleep patterns.
In summary, employing these techniques within cognitive restructuring not only aids in addressing the roots of insomnia but also empowers individuals to take an active role in their healing journey. By adapting their thoughts and behaviors, clients can create an environment conducive to restful nights.
The Impact of Cognitive Restructuring on Sleep Quality
Cognitive restructuring has a profound impact on sleep quality, particularly for those battling insomnia. By systematically addressing the underlying negative thought processes, individuals often experience a marked improvement in their ability to fall asleep and stay asleep. The reduction in sleep-related anxiety is essential in breaking the cycle of insomnia, ultimately resulting in a more restorative sleep experience.
Research indicates that individuals who engage in cognitive restructuring through cognitive-behavioral therapy typically report a decrease in sleep latency – the time it takes to fall asleep. This improvement is often attributed to the dismantling of irrational fears and the fostering of a more relaxed state of mind conducive to sleep. As they navigate these changes, clients may find themselves falling asleep faster and waking less frequently during the night.
Furthermore, the emotional benefits of cognitive restructuring extend beyond sleep quality itself. Clients often report feeling more in control of their thoughts and emotions, leading to enhanced resilience against stressors unrelated to sleep. This newfound emotional regulation can contribute to an overall increase in life satisfaction and well-being, further reinforcing positive sleep patterns.
As sleep quality improves, individuals may also notice enhancements in daytime functioning, such as increased focus, energy, and cognitive clarity. This positive feedback loop encourages clients to continue applying cognitive restructuring techniques, solidifying new habits that promote better sleep health. In essence, the cognitive shifts experienced during therapy do not just result in improved sleep; they also elevate overall quality of life.
In conclusion, the impact of cognitive restructuring on sleep quality is both multidimensional and significant. By targeting and transforming negative thought patterns, individuals with insomnia can reclaim restorative sleep, leading to lasting changes in their overall mental and emotional well-being.
3. Sleep Restriction
Understanding Sleep Restriction Therapy
Sleep restriction therapy is a cornerstone of cognitive behavioral therapy for insomnia (CBT-I). It revolves around limiting the time spent in bed to match the actual sleep time, thus creating a mild sleep deprivation that can help strengthen the body's sleep drive. The initial phase may be challenging but essential for setting a solid foundation for better sleep. Once the individual starts adhering to a restricted sleep schedule, they often notice an improvement in the quality and duration of their sleep.
The mechanism behind sleep restriction lies in the principle of sleep consolidation. By reducing the time spent in bed, individuals may experience increased sleep pressure, helping them fall asleep more quickly and stay asleep longer. This creates a new association between the bed and sleep, promoting healthier sleep habits over time. It is crucial for therapists to guide patients through this process effectively to mitigate any feelings of frustration or anxiety that may arise.
One of the key components of sleep restriction therapy is the sleep diary. Individuals are encouraged to keep meticulous records of their sleep patterns, noting the times when they go to bed, wake up, and experience nighttime awakenings. This helps in understanding their unique sleep needs and patterns, laying the groundwork for tailoring a personalized sleep schedule that fosters improved restfulness.
Moreover, the success of sleep restriction is often measured not just in terms of quantity but also quality of sleep. Research has shown that, alongside improved sleep duration, the efficiency of sleep tends to increase, meaning individuals can achieve more restorative sleep in a shorter period. This efficiency can bolster daytime alertness and overall well-being, illustrating the holistic benefits of sleep restriction therapy as part of CBT-I.
In conclusion, sleep restriction therapy serves as a pivotal strategy within cognitive behavioral therapy for insomnia, emphasizing the importance of structured sleep patterns. By adhering to a sleep schedule that aligns closely with actual sleep need, individuals start to reprogram their body’s sleep mechanisms, fostering a healthier relationship with sleep over time.
Implementing Sleep Restriction Procedures
Implementing sleep restriction procedures involves careful planning and adherence to established guidelines. Initially, patients are asked to determine their average sleep duration over a week, which helps to set a baseline. This average duration is identified from the sleep diary, enabling a precise identification of how much time should be allocated for sleep. From this information, the therapist can craft a customized sleep schedule that promotes efficiency.
The next step is to define a consistent wake-up time, which serves as a crucial component of the sleep restriction method. By waking up at the same time daily, the body can establish a reliable circadian rhythm, signaling when it's time to sleep. It is equally important to restrict the time spent in bed to match the predetermined amount of sleep, thereby avoiding the temptation to linger in bed awake, which may lead to a negative association with the sleep environment.
During this phase of therapy, individuals may encounter feelings of fatigue or irritability due to the intentional sleep deprivation created by restricting hours in bed. However, cognitive behavioral strategies, such as positive reinforcement and mindfulness techniques, can support patients in coping with these feelings effectively. Support and encouragement from therapists can also help bolster confidence during this transitional phase.
As individuals adhere to their new sleep schedule, gradual adjustments may be introduced. If sleep efficiency improves and there are fewer awakenings during the night, an individual may then increase their total time in bed in small increments. This step-wise approach allows for fine-tuning of the sleep schedule, ensuring that it remains tailored to individual needs while prioritizing improved sleep quality.
In summary, implementing sleep restriction procedures requires a structured approach, commitment, and ongoing adjustments based on observed sleep patterns. When done thoughtfully, these procedures can lead to significant improvements in sleep quality, reinforcing the effectiveness of cognitive behavioral therapy for insomnia.
Overcoming Challenges in Sleep Restriction Therapy
Despite its effectiveness, sleep restriction therapy is not without its challenges. Individuals may struggle with the initial feelings of sleep deprivation, leading to significant discomfort and reluctance to adhere to the prescribed schedule. It is crucial for therapists to prepare patients for these challenges by emphasizing the short-term discomfort may lead to long-term benefits.
Another common obstacle is anxiety related to sleep performance. Individuals may become overly focused on falling asleep quickly or maintaining uninterrupted sleep, which can paradoxically create pressure and hinder their ability to sleep. Cognitive and behavioral strategies taught in CBT-I can help patients reframe their thoughts and reduce performance anxiety, providing the tools necessary to combat these intrusive thoughts.
Maintaining the discipline required for sleep restriction may also pose a challenge, particularly when external factors, such as work schedules or social commitments, disrupt established routines. Therapists can provide guidance on how to navigate these disruptions, offering flexibility within the framework of the therapy while still maintaining the rigorous adherence that underlies sleep restriction.
Additionally, individuals may experience doubts about whether sleep restriction is actually beneficial, especially if they experience an initial dip in sleep quality before improvements manifest. Education about the science behind sleep and the rationale for the therapy is essential to foster understanding and trust in the process. Armed with knowledge, individuals can better adjust their expectations and adhere to the recommended sleep patterns.
In conclusion, while sleep restriction therapy can present challenges, these can be overcome with a solid support system and understanding of the process. By facing these obstacles head-on, individuals can ultimately reap the rewards of enhanced sleep quality and duration, contributing positively to their overall well-being.
4. Stimulus Control
Understanding Stimulus Control in CBT-I
Stimulus control is a fundamental concept within Cognitive Behavioral Therapy for Insomnia (CBT-I). At its core, it involves establishing a robust association between the bed and sleep,而 this is crucial because many people inadvertently create negative associations with their sleeping environments. For instance, working, eating, or watching television in bed can lead to mental confusion about the purpose of the sleep space, making it harder to fall asleep when truly needed.
One of the primary goals of stimulus control is to reinforce the behavior of getting into bed only when feeling sleepy. This practice helps to condition the mind, facilitating a quicker transition into sleep. When the bed is used solely for sleeping and intimacy, the brain learns to associate it with relaxation and slumber, effectively reducing the time it takes to feel sleepy and fall asleep.
Additionally, stimulus control often includes specific guidelines on when to get out of bed. If sleep doesn't occur within about 20 minutes, individuals are encouraged to leave the bedroom and engage in a calming, non-stimulating activity until they feel drowsy again. This approach minimizes the anxiety and frustration that often accompany sleeplessness, allowing the mind to reset and prepare for slumber when one returns to bed.
Over time, by consistently applying these principles, individuals can significantly improve their sleep quality and establish healthier sleep patterns. As they practice these strategies, the bed's role transforms from a site of anxiety and alertness to one of comfort and repose, ultimately fostering a more conducive environment for restorative sleep.
Clients undergoing CBT-I often find that the inclusion of stimulus control techniques plays a vital role in their journey towards better sleep. As they gain greater awareness of their sleep cues and patterns, they become empowered to take control over their sleeplessness, paving the way for a brighter, well-rested future.
Practical Strategies for Implementing Stimulus Control
Implementing stimulus control strategies requires a structured approach, blending consistency with adaptability to personal triggers. First, individuals should designate a strict sleep schedule by going to bed and waking up at the same time every day, even on weekends. This regularity reinforces the body’s circadian rhythm, making it progressively easier to fall asleep at the appropriate time.
It's also essential to create a sleep-friendly environment. This includes adjusting the room's temperature, ensuring that it is dark and quiet, and making use of comfortable bedding. By modifying the sleep environment to align with conditions that promote rest, individuals can further enhance their ability to fall asleep efficiently. Small investments in blackout curtains or white noise machines can yield significant dividends in sleep quality.
Another strategy involves identifying and eliminating sleep disruptors such as caffeine and screen time before bed. Limiting exposure to screens at least an hour before bedtime is especially crucial; the blue light emitted from devices can interfere with the body's natural production of melatonin, the hormone responsible for sleepiness. Encouraging alternative evening activities that promote relaxation, such as reading or gentle stretching, can foster a smoother transition to sleep.
As part of the stimulus control process, individuals should also reflect on their thoughts and feelings about sleep. Stress and anxiety can undermine efforts to establish healthy sleep patterns, making practices such as mindfulness meditation or deep-breathing exercises beneficial to incorporate into nightly routines. These methods can help quiet the mind and set the stage for restful slumber.
Ultimately, the effectiveness of stimulus control strategies relies on ongoing commitment. It can take time for the body and mind to adapt to these changes, but with persistence, individuals can enjoy healthier sleep and improved overall well-being.
Challenges and Solutions in Stimulus Control
Embarking on the journey of stimulus control within CBT-I brings its share of challenges, especially for those with ingrained habits. One common obstacle is the persistent temptation to stay in bed despite not feeling sleepy. This behavior is often driven by an emotional desire for rest, and can be exacerbated by the frustration that comes with insomnia. To overcome this, individuals should consciously remind themselves of the principles of stimulus control and their long-term benefits, maintaining focus on what is ultimately more restorative.
Another widespread difficulty is the inevitable disruption of sleep schedules due to life events, such as travel or work commitments. Adjusting to different time zones or late-night schedules can throw off a carefully established routine. To counteract this, it is advisable to maintain flexibility in sleep patterns while striving to revert to a regular schedule as soon as possible, reinforcing the body’s natural rhythm upon returning home.
Emotional responses can also present significant hurdles. The anxiety associated with insomnia can make individuals reluctant to adhere to stimulus control methods. Ongoing education about sleep hygiene and CBT-I can provide reassurance and pave the way for more consistent practice of techniques. Encouraging participation in support groups or therapy sessions can also create a sense of community and lessen feelings of isolation.
Moreover, cravings for late-night snacking or unhealthy habits like consuming alcohol can undermine progress in stimulus control. Here, awareness and planning are critical. Keeping healthier snacks on hand and establishing a clear boundary around eating before bed can help individuals stay aligned with their stimulus control goals.
Lastly, the process of adapting to stimulus control strategies can feel overwhelming for some. Breaking down the overall goal into smaller, manageable steps can ease this burden. Engaging with a sleep specialist or therapist familiar with CBT-I can provide invaluable guidance and ensure a more structured and supportive approach to overcoming obstacles to effective sleep management.
5. Lifestyle Adjustments
Understanding Sleep Hygiene
Sleep hygiene encompasses a series of practices and habits that are tailored to improve sleep quality and duration. It is essential to establish a daily routine that signals to your body when it is time to wind down. This includes maintaining a consistent sleep schedule, as going to bed and waking up at the same times every day can reinforce your body's natural circadian rhythms, making it easier to fall asleep and stay asleep throughout the night.
Additionally, your sleeping environment plays a critical role in sleep hygiene. The bedroom should be a sanctuary for sleep, free from distractions such as excessive noise, bright lights, and electronic devices. A cool, dark, and quiet room can enhance comfort and promote restful sleep. Routine cleaning and organizing of the space can also minimize anxiety and promote a sense of calm, allowing your mind to relax as you prepare for sleep.
Creating a Relaxation Routine
Establishing a relaxation routine before bedtime can significantly impact your ability to fall asleep. Engaging in calming activities, such as reading, practicing mindfulness meditation, or taking a warm bath, can help transition your body from the busyness of the day to a restful state. These activities can lower stress levels and signal the body that it is time to relax, making it easier to drift off into sleep.
Incorporating deep breathing exercises or gentle stretching can further enhance this relaxation routine. These practices reduce muscle tension and encourage a sense of tranquility. Engaging in such behaviors consistently can create an association between these calming activities and sleep, reinforcing healthy sleeping habits over time and contributing to the overall effectiveness of Cognitive Behavioral Therapy (CBT) techniques.
Managing Stress and Anxiety
Effective management of stress and anxiety is crucial in addressing insomnia through lifestyle adjustments. Individuals can benefit from various techniques, such as cognitive reframing, which involves reshaping negative thoughts surrounding sleep or anxiety-provoking situations. By challenging and replacing irrational beliefs with positive affirmations, individuals can cultivate a more peaceful mindset conducive to restful sleep.
In addition, incorporating regular physical activity into your daily routine can profoundly impact stress levels. Exercise releases endorphins, known as "feel-good" hormones, which promote an overall sense of well-being. Even light activities, such as walking or yoga, can help alleviate anxiety and make it easier to settle down into sleep, reinforcing the principles taught in CBT for insomnia.
Limiting Stimulants and Distractions
One significant adjustment individuals can make in their lifestyle is to limit the intake of stimulants, especially in the hours leading up to bedtime. Substances like caffeine and nicotine can significantly impact the ability to fall asleep and maintain uninterrupted sleep. Being mindful of when and how much of these substances are consumed can support a smoother transition into restful sleep.
Additionally, reducing screen time before bed is another powerful strategy. The blue light emitted by screens can interfere with the body's natural production of melatonin, a hormone that regulates sleep. By establishing a 'tech-free' zone in the hour before bed, individuals can enhance their sleep quality and responsiveness to CBT interventions targeted at insomnia, creating a more favorable sleep environment.
Engaging in Regular Sleep Tracking
Keeping a sleep diary or utilizing a sleep tracking app can be a valuable tool in understanding personal sleep patterns and identifying factors that affect sleep quality. This practice involves recording details such as bedtime, wake-up time, total sleep duration, and any disturbances experienced during the night. Gaining insights from these patterns can illuminate responsibilities related to insomnia and guide adjustments in behavior.
Moreover, sleep tracking can provide accountability and motivation in adhering to the sleep hygiene practices discussed earlier. By reviewing progress regularly, individuals can recognize improvements and setbacks, allowing for targeted changes to be made. This proactive approach can enhance the efficacy of Cognitive Behavioral Therapy techniques, leading to a more profound and lasting transformation in sleep habits.
Benefits of CBT-I
Improved Sleep Quality
Cognitive Behavioral Therapy for Insomnia (CBT-I) has been extensively studied and shown to significantly enhance sleep quality for many individuals. By addressing the thoughts and behaviors that contribute to sleep disturbances, CBT-I helps individuals learn healthier sleep patterns. This change often leads to deeper, more restorative sleep, reducing the time spent awake during the night, and allowing the body to adequately recover and rejuvenate.
Many participants in CBT-I programs report not only falling asleep quicker but also experiencing fewer awakenings throughout the night. This improvement doesn't just enhance nighttime rest; it also translates into better performance and mood during the day. With increased energy levels and cognitive function, people can engage more fully in daily activities and responsibilities, leading to an overall improved quality of life.
Long-term Effectiveness
One of the remarkable advantages of CBT-I is its long-term effectiveness in treating insomnia. Unlike medication, which often addresses symptoms transiently and can lead to dependency, CBT-I equips individuals with essential self-help skills and tools to manage and prevent future sleep issues. This approach fosters a deeper understanding of personal sleep patterns and the emotional and cognitive triggers that impact rest.
Studies show that individuals who undergo CBT-I have sustained improvements in their sleep quality even after completing the therapy. This means that the benefits extend well beyond the therapy sessions, empowering individuals to maintain healthier sleep practices over time. Such resilience against future insomnia can lead to fewer healthcare costs associated with sleep disorders and the challenges they present.
Reduction of Anxiety and Depression Symptoms
CBT-I not only targets the mechanics of sleep but is also effective in alleviating symptoms associated with anxiety and depression. Sleep disturbances are often linked to mental health issues, creating a vicious cycle where one exacerbates the other. CBT-I addresses this intersection by helping individuals manage their thoughts and worries, which contributes to both better sleep and improved mental health.
Personal Empowerment and Self-Management
Through CBT-I, individuals gain invaluable skills in managing their sleep health, leading to a sense of empowerment and control over their lives. The techniques learned, such as sleep hygiene practices and cognitive restructuring, promote proactive self-management. This empowerment allows individuals to anticipate and tackle sleep challenges that may arise in the future.
As participants become adept in applying these strategies, they often report an increased confidence in their ability to achieve restful sleep without relying solely on pharmaceuticals. This newfound agency fosters a healthier relationship with sleep, leading to an overall improved lifestyle that prioritizes well-being and self-care. By breaking the cycle of insomnia, individuals can cultivate a more peaceful and fulfilling daily existence.