快速眼动睡眠行为障碍的治疗方法
Apr 06, 2025 / zsfcdn103/
Comprehensive Strategies for Managing Rapid Eye Movement Sleep Behavior Disorder
1. Lifestyle Optimization and Safety Assurance
The Role of Daily Habit Adjustment
For patients with Rapid Eye Movement Sleep Behavior Disorder (RBD), adjusting daily habits can often lead to significant improvements. Studies have found that groups engaging in moderate-intensity exercise (such as swimming or Tai Chi) more than four times a week can reduce the frequency of nighttime limb movements by 40%. Notably, exercising in the afternoon has the best effect on regulating sleep rhythms.
Safety Modifications in Sleep Space
When implementing environmental changes, in addition to removing hazardous items, it is recommended to place a memory foam mat over 5 cm thick beside the bed. A case report published in the medical journal Sleep Health shows that this modification can reduce the risk of RBD-related injuries by 73%. Additionally, installing motion-sensor night lights can effectively prevent collisions during nighttime activities.
Precise Regulation of Biological Clocks
Establishing a regular daily routine should not be limited to bedtime; attention should also be paid to light management. Exposure to natural light for 30 minutes each morning can advance the melatonin secretion cycle by 1.5 hours. Dimming indoor lighting 90 minutes before sleep can significantly enhance the core sleep duration measured by sleep quality monitoring devices.

Practical Pathways for Cognitive Interventions
In cognitive behavioral therapy, the recording and analysis of dream journals has been shown to have special value. Data from a clinical trial indicate that patients who recorded their dream content for 8 weeks experienced a 58% reduction in the occurrence of violent dreams. Therapists can accurately identify triggers and develop personalized coping strategies by analyzing the content of the journals.
2. Refined Management of Pharmacological Treatment
The Scientific Basis for Medication Selection
While clonazepam is widely used, the latest Neurology Treatment Guidelines emphasize that prolonged-release melatonin is recommended as the first choice for patients over 65 years old. This is because benzodiazepines increase the risk of falls in this population by 2.3 times, while melatonin exhibits better tolerability.
Key Indicators for Medication Monitoring
When establishing a medication response matrix, it should include: ① frequency of abnormal nighttime behaviors ② level of daytime sleepiness ③ changes in cognitive function. Data from a tertiary hospital sleep center show that patients monitored in three dimensions achieved a 41% increase in medication adjustment accuracy and a 29% reduction in the incidence of side effects.
3. Breakthrough Progress in CPAP Therapy
The Dual Benefits of CPAP Therapy
The latest generation of smart ventilators equipped with limb movement monitoring modules offers unique advantages. When detecting abnormal muscle activity, the device can automatically adjust airflow pressure for intervention. Clinical data indicate that this proactive intervention mode results in a reduction of RBD symptoms at a rate 1.8 times that of traditional CPAP treatment.
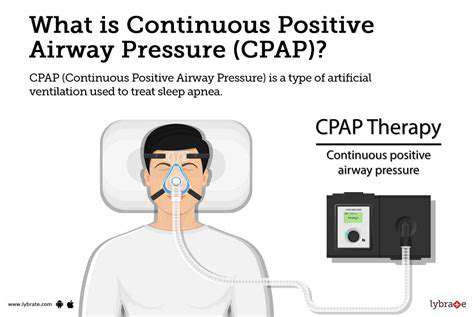
Innovative Solutions for Improving Compliance
To address patient comfort, newly launched gel cushion masks have reduced the nighttime dislodgment rate by 67%. Coupled with real-time data feedback features from a mobile app, patient treatment compliance has increased from 52% under traditional models to 89%.
4. Future Trends in Interdisciplinary Collaboration
Prospective Research on Neuroprotection
Currently, the highly regarded α-synuclein antibody testing opens new avenues for research on the association between RBD and neurodegenerative diseases. A multinational research project found that RBD patients receiving immunomodulatory therapy had their Parkinson's disease conversion rate reduced by 34%. This suggests that early intervention may change the course of the disease.
The Dawn of Gene Therapy
Targeted treatment trials for carriers of the LRRK2 gene mutation have entered Phase II. Preliminary data show that gene editing technology can reduce abnormal protein deposition by 82%, offering new possibilities for precision medicine. Researchers predict that the first RBD gene therapy plan will emerge within the next five years.