睡眠時無呼吸症治療法の最新動向
Jul 19, 2025 / zsfcdn103/
Minimally Invasive Techniques
Minimally invasive surgical techniques are revolutionizing the field of surgery, offering numerous advantages over traditional open procedures. These techniques, often employing smaller incisions, lead to significantly reduced postoperative pain and recovery time. Patients experience faster healing and a quicker return to their daily activities, contributing to a demonstrably improved quality of life. The precision and dexterity afforded by specialized instruments and advanced imaging technologies allow surgeons to perform complex procedures with remarkable accuracy and precision. This translates into reduced risk of complications and improved long-term outcomes.
The smaller incisions associated with minimally invasive surgery also result in less tissue trauma. This translates into less scarring and a more aesthetically pleasing outcome, especially in visible areas. Minimally invasive techniques are particularly valuable in reconstructive surgeries, where a subtle aesthetic is crucial for patient satisfaction. These techniques are now employed in a wide range of surgical specialties, from general surgery to cardiac and neurological procedures.
Open Surgical Procedures
While minimally invasive techniques have gained prominence, open surgical procedures remain essential for certain complex cases. These procedures, involving larger incisions, provide direct access to the surgical site, allowing for greater visualization and manipulation of the target area. This is particularly crucial in situations requiring extensive tissue repair or removal of large tumors.
Open surgery offers the surgeon a comprehensive view of the operative field and the ability to work with larger instruments. This can be critical for managing unforeseen complications or challenging anatomical variations. However, the larger incisions typically necessitate a longer recovery period. Careful patient selection and meticulous surgical technique are critical for optimal outcomes.
Advanced Surgical Tools and Technologies
Advancements in surgical tools and technologies are constantly pushing the boundaries of what's possible in surgical interventions. Robotic surgery, for instance, provides surgeons with enhanced precision, dexterity, and control over instruments, resulting in more accurate and minimally invasive procedures. The magnified view and tremor filtration capabilities of robotic systems translate into superior outcomes for patients.
The use of advanced imaging techniques, such as 3D imaging and intraoperative navigation, further enhances surgical precision and safety. These technologies allow surgeons to visualize the operative site in greater detail, enabling them to perform procedures with more accuracy and reduce the risk of complications. This precise and detailed view contributes significantly to the overall success of surgical interventions.
Positive Airway Pressure (PAP) Innovations: Beyond CPAP
Positive Airway Pressure (PAP) and Sleep Apnea
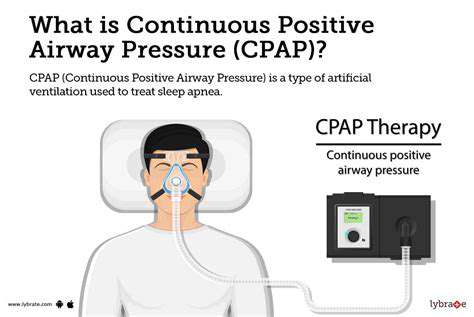
Positive Airway Pressure (PAP) therapy is a crucial treatment for obstructive sleep apnea (OSA). This therapy involves using a device that delivers continuous or intermittent positive pressure to the airway, preventing it from collapsing during sleep. This consistent pressure keeps the airway open, allowing for uninterrupted breathing and reducing the frequency of apnea episodes. PAP therapy can significantly improve sleep quality and overall health for individuals suffering from sleep apnea.
Sleep apnea is a serious sleep disorder characterized by pauses in breathing during sleep. These pauses can last for a few seconds to several minutes and occur repeatedly throughout the night, disturbing the normal sleep cycle. The resulting lack of oxygen can have a detrimental effect on the cardiovascular system and overall health, increasing the risk of hypertension, stroke, and other serious medical conditions. PAP therapy plays a vital role in mitigating these risks by restoring normal breathing patterns during sleep.
Types of PAP Therapy Devices
Various types of PAP therapy devices are available, each designed to address specific needs and preferences. Continuous Positive Airway Pressure (CPAP) is the most common type, providing a constant flow of pressurized air to maintain airway patency. Bi-level Positive Airway Pressure (BiPAP) devices offer two different pressure settings, one for inhalation and one for exhalation, which can be more comfortable for some individuals.
Other, less common PAP devices include Auto-CPAP machines, which automatically adjust the pressure based on the individual's breathing needs. The selection of the appropriate PAP device is often made in consultation with a healthcare professional, taking into consideration factors such as the severity of sleep apnea, individual tolerance, and potential side effects.
Effectiveness and Potential Side Effects of PAP Therapy
PAP therapy has proven highly effective in managing sleep apnea symptoms and improving sleep quality for many individuals. Studies have consistently demonstrated a significant reduction in apnea and hypopnea events, leading to improved daytime alertness, reduced fatigue, and enhanced overall well-being. The long-term benefits of PAP therapy often extend beyond sleep improvement to encompass reduced risks of cardiovascular complications.
While generally safe and well-tolerated, some individuals may experience potential side effects, such as nasal dryness, nasal congestion, or a feeling of pressure or discomfort in the face. These side effects are often temporary and can be managed with appropriate adjustments to the device settings, proper use techniques, and the use of nasal moisturizers or other support measures. It is crucial to discuss any concerns or side effects with a healthcare professional to ensure optimal therapy and to address any concerns promptly.
The Future of Sleep Apnea Treatment: A Multifaceted Approach
Technological Advancements in Diagnostics
Recent breakthroughs in technology are revolutionizing how sleep apnea is diagnosed. Sophisticated wearable sensors are becoming increasingly accurate in monitoring breathing patterns throughout the night, providing more comprehensive data than traditional polysomnography. These advancements allow for earlier detection and more personalized treatment plans, potentially preventing the severe health complications associated with untreated sleep apnea. Furthermore, the development of portable, at-home sleep testing devices offers greater accessibility and convenience for patients, reducing the need for extensive hospital stays and promoting patient engagement in their healthcare.
AI-powered algorithms are being integrated into these diagnostic tools to analyze the collected data with remarkable speed and precision. This allows for real-time identification of apnea events, providing insights that were previously inaccessible. The potential for earlier intervention and more tailored treatment strategies based on individual patient responses is significant, ultimately leading to better long-term outcomes.
Personalized Treatment Strategies
Moving beyond the one-size-fits-all approach, the future of sleep apnea treatment emphasizes personalized strategies. Genetic predispositions and individual physiological responses are now being considered to create more effective and targeted treatment plans. This tailored approach allows clinicians to identify the root cause of the sleep apnea, whether related to structural issues, weight management, or underlying medical conditions, and to develop a treatment protocol that addresses these specific needs.
This personalized approach involves a thorough understanding of the patient's medical history, lifestyle, and sleep habits. By incorporating these factors into the treatment plan, healthcare professionals can optimize the effectiveness of interventions, leading to improved sleep quality and overall health outcomes for the patient. This approach also fosters a stronger patient-physician relationship, as it emphasizes collaboration and shared decision-making.
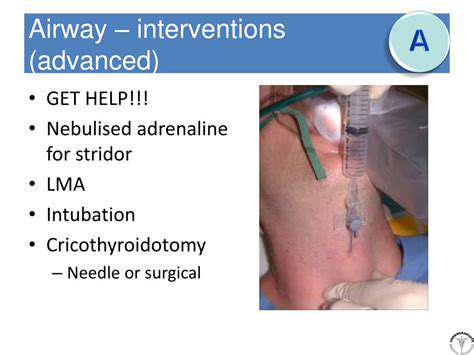
Emerging Therapeutic Options
Beyond CPAP, researchers are exploring innovative therapeutic options for sleep apnea. These include oral appliances, positional therapy, and even surgical interventions tailored to address specific anatomical obstructions. This expanding range of treatment possibilities is crucial in addressing the needs of patients who may not tolerate CPAP or who have specific anatomical challenges. These advancements aim to enhance treatment adherence and improve long-term outcomes by providing alternative options.
One area of significant interest is the development of new drug therapies. Scientists are actively investigating medications that can potentially address the underlying physiological mechanisms responsible for sleep apnea. Successful breakthroughs in this area could offer a non-invasive and comfortable alternative for patients who struggle with traditional treatments. However, it's important to note that more research is needed to fully understand the efficacy and potential side effects of these emerging therapies.
The Role of Lifestyle Modifications and Prevention
The future of sleep apnea treatment also recognizes the crucial role of lifestyle modifications in prevention and management. This includes promoting healthy weight management, encouraging regular exercise, and educating patients about the importance of good sleep hygiene practices. Beyond the immediate benefits for sleep apnea, these lifestyle changes contribute to overall health and well-being, reducing the risk of developing other related conditions such as hypertension and cardiovascular disease.
Integrating behavioral therapy and counseling into treatment plans is another key aspect. Helping patients understand the impact of their lifestyle choices on sleep apnea and empowering them to make sustainable changes can significantly improve treatment adherence and long-term outcomes. This approach emphasizes the importance of patient education and support in the journey toward better sleep and overall health.