CPAPマシンの医療用途の理解
May 09, 2025 / zsfcdn103/
Sleep apnea, a condition marked by repeated breathing interruptions during sleep, has emerged as a major contributor to various heart-related illnesses. The repeated oxygen deprivation caused by sleep apnea throws the body's regulatory systems into disarray, creating a domino effect of harmful consequences for heart health. These disruptions often lead to elevated blood pressure, heightened inflammation, and compromised blood vessel function - all precursors to serious conditions like high blood pressure, clogged arteries, and strokes.
While researchers continue to unravel the precise biological mechanisms, the relationship between sleep apnea and heart disease has been firmly established. Multiple clinical investigations have shown that the more severe a person's sleep apnea, the greater their likelihood of developing cardiovascular issues. Recognizing this connection is vital for implementing protective measures and appropriate treatments.
The Role of Intermittent Oxygen Deprivation
At the heart of the sleep apnea-cardiovascular connection lies the pattern of recurring oxygen deprivation. These periodic drops in oxygen supply trigger widespread inflammation throughout the body. This inflammatory reaction damages arterial walls, accelerates plaque accumulation in blood vessels, and sets the stage for atherosclerosis - the primary culprit behind most heart disease.
The constant yo-yoing of oxygen levels places extraordinary stress on the cardiovascular system, forcing the heart and blood vessels to work harder. Over time, this strain frequently results in chronic high blood pressure, which independently raises the risk of heart attacks and other cardiovascular emergencies.
Disruption of Blood Pressure Control
Sleep apnea wreaks havoc on the body's natural ability to regulate blood pressure. The frequent nighttime awakenings and gasping for air cause wild blood pressure swings that often evolve into persistent hypertension. This sustained high blood pressure overworks the heart and damages blood vessels, dramatically increasing the chances of heart attacks, strokes, and other serious complications.
What makes sleep apnea particularly dangerous is its tendency to go undetected for years, allowing cardiovascular damage to progress unchecked. Identifying and treating sleep disorders early could prevent countless cases of heart disease.
Inflammation and Cellular Damage
The oxygen deprivation caused by sleep apnea sparks widespread inflammation, evident in elevated inflammatory markers circulating in the bloodstream. This persistent inflammatory state impairs the function of blood vessel linings. This endothelial dysfunction represents a critical step in the development of atherosclerosis and subsequent heart disease.
Additionally, sleep apnea generates oxidative stress - a process that damages cells through harmful molecules called free radicals. This oxidative damage worsens inflammation and further compromises blood vessel function, creating a vicious cycle that accelerates cardiovascular decline.
Blood Vessel Lining Damage
The impairment of endothelial cells lining blood vessels forms a crucial link between sleep apnea and heart disease. The erratic oxygen supply caused by breathing interruptions during sleep injures these delicate cells, promoting blood clot formation and inflammation. This damaged endothelial layer significantly contributes to artery clogging and the cardiovascular events that follow.
Treatment and Prevention Approaches
Given the clear connection between sleep apnea and heart disease, aggressive treatment and prevention strategies are essential. Early detection and proper management of sleep apnea through CPAP therapy or other treatments can dramatically reduce cardiovascular risks. Lifestyle changes including weight management, consistent physical activity, and heart-healthy eating patterns can also improve cardiovascular health while potentially lessening sleep apnea severity.
Increasing public awareness about sleep apnea symptoms could prompt more people to seek evaluation, leading to earlier diagnosis and treatment. This comprehensive approach offers the best chance for protecting heart health and preventing related complications.
Breach of trust brings emotional wounds to intimate relationships that are difficult to heal.
Important Considerations and Precautions
Understanding the Potential Benefits
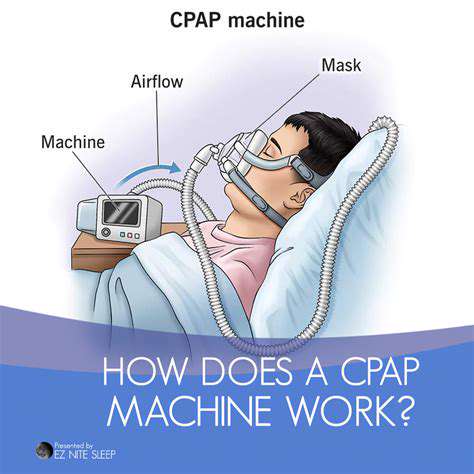
CPAP therapy, which delivers continuous air pressure, provides numerous advantages for people with obstructive sleep apnea. By keeping airways open throughout the night, CPAP prevents breathing pauses, ensuring proper oxygen levels and reducing sleep disruptions. This leads to more restorative sleep and better daytime functioning.
Patients often notice dramatic improvements in daytime energy, mental clarity, and overall quality of life when using CPAP consistently. These benefits can transform work performance, personal relationships, and general wellbeing.
Addressing Potential Side Effects
While generally safe, CPAP can sometimes cause nasal irritation, dryness, or minor discomfort. These issues are usually temporary and can be managed through proper humidification, mask adjustments, or nasal saline solutions.
Any persistent problems should be discussed with a sleep specialist, who can recommend solutions tailored to individual needs and preferences.
Proper Mask Selection and Fit
Choosing the right mask style (nasal, full-face, or nasal pillows) and ensuring proper fit are critical for treatment success. A well-fitted mask prevents air leaks while remaining comfortable throughout the night.
Sleep professionals can help patients test different mask options to find the most comfortable and effective solution for their unique facial structure and sleeping habits.
Maintaining Consistent Use
Regular CPAP use is essential for achieving maximum benefits. Consistent nightly use helps regulate breathing patterns, improves sleep quality, and reduces health risks associated with sleep apnea.
Patients struggling with compliance should work with their healthcare team to identify and address any barriers to regular use.
Understanding Pressure Settings
CPAP devices feature customizable pressure levels determined through sleep studies. Proper pressure settings ensure airways remain open without causing discomfort or excessive dryness.
Importance of Regular Follow-up Appointments
Ongoing medical supervision helps optimize CPAP therapy over time. Follow-up visits allow for pressure adjustments, mask refitting, and troubleshooting of any issues that may arise during treatment.
These check-ins also provide opportunities to discuss treatment progress and make any necessary modifications to the care plan.