探索正压通气治疗方案
Jul 07, 2025 / zsfcdn103/
Positive airway pressure (PAP) ventilation is a crucial respiratory support technique employed in various clinical settings to assist or maintain adequate ventilation. This method involves delivering a continuous or intermittent positive pressure into the airway, thereby expanding the lungs and facilitating gas exchange. Understanding the mechanics and applications of PAP ventilation is essential for healthcare professionals involved in patient care.
PAP ventilation is a cornerstone of respiratory therapy, offering a wide range of applications for treating various respiratory conditions. Its precise use and careful monitoring are critical to ensuring patient safety and efficacy.
Types of PAP Ventilation
Different types of PAP ventilation devices and modes exist, each tailored to specific patient needs and respiratory conditions. Continuous positive airway pressure (CPAP) is a common example, providing a constant level of positive pressure throughout the respiratory cycle. This is often used for obstructive sleep apnea.
Another type is bi-level positive airway pressure (BiPAP), which delivers different levels of positive pressure during inspiration and expiration. This offers more flexibility in adjusting pressure based on individual patient requirements.
These variations provide a range of therapeutic options, each with its own set of advantages and disadvantages. Selecting the appropriate type and settings is crucial for optimal patient outcomes.
Mechanism of Action
The fundamental mechanism of PAP ventilation involves increasing the pressure within the airway. This elevated pressure counteracts the forces of airway collapse and improves lung expansion. The increased lung volume allows for more effective gas exchange, leading to better oxygenation and carbon dioxide removal.
This pressure support directly impacts the mechanics of breathing, making it easier for the patient to inhale and exhale. By overcoming resistance in the airways, PAP ventilation facilitates better ventilation and oxygenation of the lungs.
Indications for Use
Positive airway pressure ventilation finds applications in a diverse range of respiratory conditions. It's commonly used for patients with acute respiratory distress syndrome (ARDS) to support lung function and oxygenation. Furthermore, it's employed to treat obstructive sleep apnea, improving sleep quality and reducing cardiovascular risks.
Other indications include chronic obstructive pulmonary disease (COPD) exacerbations, and in the postoperative period for patients requiring respiratory support. The use of PAP ventilation is carefully evaluated based on individual patient conditions and needs.
Potential Complications and Considerations
While generally safe, PAP ventilation can present potential complications, such as pneumothorax, barotrauma, and mask discomfort. Careful monitoring of the patient's respiratory status, hemodynamic stability, and overall response to the therapy is critical. Appropriate mask fitting and patient education are paramount to minimize discomfort and ensure the device's effectiveness.
Proper training and expertise in the management of PAP ventilation are essential to minimize potential risks and maximize patient benefit. Potential complications must be recognized and addressed promptly to ensure patient safety.
Types of PAP Therapy Devices
Types of PAP Therapy Devices
Positive airway pressure (PAP) therapy devices are crucial for managing sleep apnea and other respiratory conditions. They work by delivering a constant flow of pressurized air to keep the airways open during sleep. Understanding the different types available can help patients and healthcare providers choose the best option for individual needs and preferences.
Different types of PAP machines offer varying levels of customization and features. This allows for a tailored approach to treatment, promoting better sleep quality and overall health outcomes. Patients should discuss the various options with their doctor to determine the most suitable device for their specific condition.
CPAP Machines
Continuous positive airway pressure (CPAP) machines are the most common type of PAP therapy device. They deliver a constant level of air pressure throughout the entire night, maintaining a stable airway opening. CPAP therapy is often the first-line treatment for obstructive sleep apnea. This consistent pressure helps to prevent airway collapse during sleep, allowing for better breathing and improved sleep quality.
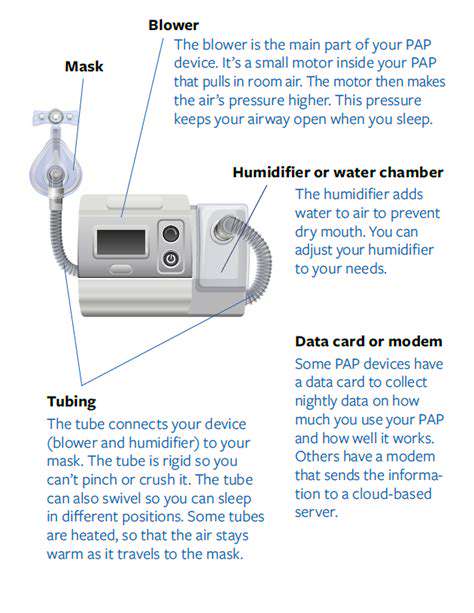
CPAP machines typically include a mask, a hose, and a pressure-regulating device. The mask is carefully selected to fit the patient's face and nose and mouth configuration. The pressure level is adjusted based on the patient's individual needs and is often monitored and adjusted by a sleep specialist.
BiPAP Machines
Bi-level positive airway pressure (BiPAP) machines offer two different pressure settings. One pressure is delivered during inhalation, and a lower pressure during exhalation. This bi-level approach can be more comfortable for some individuals compared to CPAP, especially those with certain respiratory conditions or those who find the constant pressure of CPAP uncomfortable. BiPAP machines offer greater flexibility in pressure settings, potentially allowing for more personalized treatment.
BiPAP machines are particularly beneficial for patients with certain respiratory issues, such as those experiencing difficulty with exhalation or those who require more pressure support during specific stages of breathing. The adjustable pressure settings provide a more adaptable approach to manage diverse respiratory needs.
APAP Machines
Auto-adjusting positive airway pressure (APAP) machines automatically adjust the pressure level throughout the night. This adaptability is based on the patient's breathing patterns and needs, providing a more comfortable and personalized experience. The ability of APAP to automatically adjust pressure can lead to a more natural sleep experience. The device continuously monitors and fine-tunes the pressure needed to keep the airways open.
APAP machines are often preferred by patients who find CPAP or BiPAP slightly uncomfortable. The automated adjustment offers a more responsive and personalized approach to airway support during sleep. They are often used for initial treatment and to help patients adapt to PAP therapy.
The Importance of Professional Guidance
Seeking Expert Advice for Optimal Outcomes
Navigating the complexities of positive airway pressure (PAP) therapy can be challenging. Understanding the various types of PAP devices, their functionalities, and the optimal settings for individual needs requires specialized knowledge. A qualified healthcare professional, such as a pulmonologist, sleep physician, or respiratory therapist, plays a crucial role in guiding patients through this process. Their expertise ensures personalized treatment plans, minimizing potential complications and maximizing the effectiveness of PAP therapy in improving sleep quality and overall health.
Seeking professional guidance extends beyond the initial prescription. Regular follow-up appointments allow for adjustments to the therapy based on individual responses and evolving health conditions. This ongoing support ensures the treatment remains tailored to the patient's specific needs, preventing frustration and maximizing the positive impact of PAP therapy on their overall well-being. It allows for early identification of potential issues and proactive interventions, ensuring the best possible results.
Personalized Treatment Plans and Long-Term Support
A key benefit of professional guidance lies in the creation of personalized treatment plans. Each individual responds differently to PAP therapy, and a healthcare professional can tailor the device type, pressure settings, and mask selection to optimize comfort and effectiveness. This individualized approach is essential for achieving optimal results and minimizing any discomfort or side effects that might arise from inappropriate treatment.
Beyond the initial consultation, ongoing support is critical for long-term adherence to PAP therapy. Regular check-ups and adjustments to the treatment plan ensure that the therapy remains effective and that any evolving health conditions are addressed. This proactive approach fosters a partnership between the patient and healthcare provider, empowering the patient to actively participate in their treatment and achieve better outcomes.
Professional guidance also encompasses education and support. Healthcare professionals can explain the benefits of PAP therapy, address patient concerns, and provide resources for ongoing support. This comprehensive approach ensures that patients are well-informed, empowered, and more likely to adhere to their treatment plan, leading to improved sleep quality and overall health.
Ultimately, professional guidance is essential for maximizing the potential benefits of PAP therapy while minimizing potential risks. This personalized approach, coupled with ongoing support, fosters a collaborative environment where patients can achieve optimal outcomes and lead healthier lives.
Expert advice not only ensures that the correct equipment and settings are used but also provides ongoing support and education, critical for long-term success with PAP therapy.