CPAP装置なしの次世代睡眠時無呼吸症候群治療法
Jul 10, 2025 / zsfcdn103/

CPAP Mask Discomfort and Leakage
One of the most common complaints among CPAP users is mask discomfort. The pressure from the mask, the fit, and the materials used can all contribute to a variety of issues, from skin irritation and pressure points to headaches and facial pain. Mask leakage is another significant frustration, often leading to poor sleep quality and reduced treatment effectiveness. Finding the right mask type and size, and practicing proper mask application techniques, are crucial steps in managing this issue.
The Noise and Annoying Sounds
The continuous whirring sound of the CPAP machine can be disruptive and distracting, making it difficult to fall asleep and stay asleep. This constant noise can be particularly problematic for individuals who are sensitive to sound or who share a bedroom with others. Some CPAP machines are quieter than others, and using a white noise machine or earplugs can also help to mitigate the problem.
Difficulty in Adjusting the Pressure Setting
Finding the right CPAP pressure setting can be a trial-and-error process. A pressure that is too high can cause discomfort, while a pressure that is too low may not adequately treat the sleep apnea. It's vital to follow the recommendations of your healthcare provider and to work closely with your sleep specialist to adjust the pressure as needed to achieve optimal results. This process may involve multiple adjustments and visits to ensure the most effective pressure setting is achieved.
Time-Consuming Set-Up and Cleaning
CPAP machines and masks require regular cleaning to prevent the growth of bacteria and mold, which can lead to respiratory infections. The process can be somewhat time-consuming and tedious, especially if you have to take apart and clean multiple components. Regular maintenance is essential for maintaining machine performance and preventing potential health risks, but the effort can still be a significant factor in the overall experience for some users.
Compliance and Consistency Issues
Maintaining consistent use of the CPAP machine is vital for effective treatment of sleep apnea. However, many patients struggle with compliance, either due to mask discomfort, the noise of the machine, or simply the inconvenience of using the device every night. Consistency is key to achieving the therapeutic benefits of CPAP therapy, and overcoming these obstacles is a significant challenge for many patients. Enlisting the support of healthcare professionals and support groups can significantly improve compliance.
Cost and Insurance Coverage
The initial cost of a CPAP machine and the ongoing expenses associated with supplies like masks and tubing can be a significant financial burden for some individuals. The cost of the equipment and associated supplies can be prohibitive for some patients, limiting access to an effective treatment. While many insurance companies cover CPAP therapy, it's important to understand your coverage and associated co-pays to avoid financial surprises. Insurance coverage and financial assistance programs can significantly reduce the financial burden associated with CPAP therapy.
Oral Appliances: A Discreet and Often Effective Option
Oral Appliances: A Discreet Approach
Oral appliances, often referred to as mandibular advancement devices (MADs), are a discreet and non-invasive approach to treating sleep apnea. Unlike CPAP machines, which require significant lifestyle adjustments, oral appliances are often more easily integrated into daily routines. They work by gently repositioning the lower jaw and tongue, opening the airway and preventing the collapse that leads to breathing interruptions during sleep. This subtle shift in the jaw's position can significantly improve airflow and reduce the severity of sleep apnea episodes.
Effectiveness and Types of Oral Appliances
The effectiveness of oral appliances in treating sleep apnea varies depending on the individual and the severity of the condition. For mild to moderate cases, oral appliances can be highly effective in reducing apnea and hypopnea events, improving sleep quality, and alleviating daytime sleepiness. Different types of appliances exist, each designed to address specific anatomical features and jaw positions. Some appliances focus on advancing the lower jaw, while others concentrate on repositioning the tongue or both.
A qualified dentist or sleep specialist can assess your specific needs and recommend the most suitable oral appliance for your condition. They can also monitor the effectiveness of the appliance and adjust it as needed to optimize its performance.
Comfort and Patient Compliance
Patient comfort and compliance are crucial factors in the success of oral appliance therapy. While some individuals experience initial discomfort, it typically subsides with time and adjustment. Many patients report that the appliances are relatively comfortable to wear throughout the night, and the benefits of improved sleep far outweigh any initial discomfort. Proper fitting and ongoing adjustments by a dental professional play a vital role in maintaining comfort and ensuring the appliance remains effective.
Cost-Effectiveness and Accessibility
Oral appliances are often a more cost-effective option compared to CPAP therapy, particularly in the long term. While the initial cost of the appliance may vary, the ongoing expenses are generally lower than the cost of CPAP supplies, such as masks and tubing. Furthermore, oral appliances are readily accessible. Many dentists are trained in sleep apnea treatment and can provide these appliances, often in a more convenient location than sleep clinics.
Potential Side Effects and Considerations
As with any medical intervention, potential side effects can occur with oral appliance therapy. Some individuals may experience minor jaw or muscle soreness in the initial stages. However, these side effects are usually temporary and resolve with continued use and potential adjustments by a dental professional. It's essential to discuss potential side effects and any concerns with your dentist or sleep specialist before starting treatment. Additionally, proper oral hygiene practices are crucial to prevent any potential dental issues related to appliance use.
Long-Term Management and Maintenance
Long-term management of sleep apnea with oral appliances involves regular check-ups with your dentist to ensure proper fit and continued effectiveness. The dentist can adjust the appliance as needed to maintain optimal airway positioning. Proper oral hygiene, including brushing and flossing around the appliance, is essential to prevent oral health problems. Regular communication with your dental professional is vital for maintaining the appliance's efficacy and addressing any emerging issues.
Positive Airway Pressure (PAP) Systems Beyond CPAP: Exploring the Latest Innovations
Bi-Level Positive Airway Pressure (BiPAP)
Bi-Level Positive Airway Pressure (BiPAP) systems offer a more tailored approach to positive airway pressure therapy compared to traditional continuous positive airway pressure (CPAP). Instead of delivering a constant pressure, BiPAP provides two different pressures: an inspiratory pressure (higher) and an expiratory pressure (lower). This allows for more natural breathing patterns, potentially making it more comfortable for some patients, particularly those with more complex sleep apnea or those experiencing difficulty transitioning from CPAP to a more advanced therapy. The adjustable pressures can be optimized to address specific breathing challenges, potentially improving overall sleep quality and reducing the risk of side effects.
BiPAP can be particularly beneficial for patients who experience CPAP-related issues like mask leaks or difficulty with the constant pressure. The variable pressure delivery can help to reduce these problems. Further, the added flexibility in pressure settings can make BiPAP a valuable option for patients with more severe sleep apnea, or for those who are struggling with the initial adaptation to positive airway pressure therapy.
Auto-Adjusting PAP Systems
Auto-adjusting PAP systems take the concept of individualized pressure delivery to the next level. These advanced devices automatically adjust the pressure throughout the night based on the patient's breathing patterns and needs. This continuous monitoring and adaptation ensures that the most effective pressure is delivered at all times. The system continuously evaluates and modifies the pressure settings, leading to a more personalized and comfortable sleep experience.
Auto-adjusting PAP systems often improve patient compliance by reducing the discomfort associated with fixed pressure settings. The system's ability to adapt to evolving breathing needs can result in a more effective treatment strategy, potentially improving sleep quality and reducing the severity of sleep apnea symptoms. This continuous adjustment can lead to a more natural and comfortable breathing experience compared to the fixed pressure of CPAP or BiPAP.
Adaptive Servo Ventilation (ASV)
Adaptive Servo Ventilation (ASV) systems represent a further step in the evolution of PAP technology. ASV is designed for patients with more complex sleep apnea, or those who have not responded adequately to standard PAP therapies. ASV systems use advanced algorithms to adjust the pressure and ventilation settings in response to the patient's breathing patterns, providing more sophisticated support for breathing during sleep. This dynamic approach is particularly valuable for those who may have difficulty maintaining adequate airflow.
ASV systems offer a personalized approach to ventilation, adapting to the unique breathing characteristics of each individual patient. By providing a more dynamic response to changing breathing patterns, ASV can potentially address underlying issues that may not be adequately addressed by other forms of PAP therapy. This tailored approach to ventilation can lead to better treatment outcomes and potentially improved sleep quality compared to other PAP options.
Oral Appliances and Mandibular Advancement Devices
While not strictly PAP systems, oral appliances and mandibular advancement devices are often used in conjunction with or as an alternative to PAP therapy. These devices are custom-fitted mouthpieces that reposition the jaw and tongue, opening the airway and preventing airway collapse during sleep. The success rate of these devices in treating mild to moderate sleep apnea is notable. They provide an alternative for individuals who may find PAP therapy uncomfortable or prefer a non-invasive approach.
These devices often offer a cost-effective and minimally invasive solution compared to PAP therapy, and they can be particularly beneficial for certain patient populations. The potential for improved sleep quality and reduced symptoms of sleep apnea makes them a valuable option for consideration. However, their effectiveness varies depending on the severity of sleep apnea and individual patient factors.
Hypoglossal Nerve Stimulation: A Promising Neuromodulation Approach
Hypoglossal Nerve Stimulation: An Overview
Hypoglossal nerve stimulation (HNS) is a relatively new therapeutic approach that involves electrically stimulating the hypoglossal nerve, which controls tongue movement. This stimulation can have a variety of effects, and is currently being explored for its potential in treating various neurological and medical conditions. Understanding the mechanisms behind HNS is crucial for appreciating its potential applications.
The hypoglossal nerve plays a critical role in voluntary movements of the tongue. Stimulating this nerve can lead to a range of responses, from subtle adjustments in tongue position to more pronounced contractions. Understanding these responses is key to tailoring stimulation protocols for specific therapeutic goals.
Mechanism of Action
The precise mechanism of action behind HNS is still under investigation, but it's believed to involve modulating neural activity in the brain regions that control tongue movement and other associated functions. This modulation can influence various physiological processes, potentially leading to therapeutic benefits.
By electrically stimulating the hypoglossal nerve, we can potentially influence the activity of connected neural pathways, leading to changes in motor output and potentially, improvements in symptom presentation.
Potential Therapeutic Applications
The potential therapeutic applications of HNS are diverse, spanning various neurological and medical conditions. One area of focus is in treating dysphagia, difficulty swallowing. By stimulating the hypoglossal nerve, it's possible to improve tongue function, leading to improved swallowing ability.
Another promising area involves treating neurological disorders impacting speech production. HNS may potentially assist in improving the articulation of speech sounds, particularly those requiring precise tongue movements. Further research is crucial to confirm these potential benefits.
Safety and Side Effects
Like any medical intervention, HNS carries potential risks and side effects. Careful consideration of the patient's medical history and potential complications is essential before initiating treatment. The most common side effects are typically mild and transient, like discomfort or temporary changes in tongue sensation.
Careful monitoring during and after stimulation is crucial to ensure the safety and well-being of the patient. Close collaboration between medical professionals and patients is essential throughout the process to address any concerns and manage potential side effects effectively.
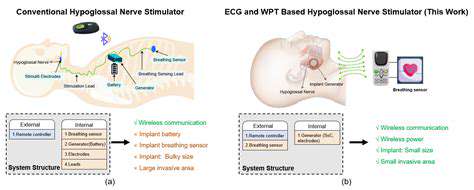
Surgical Procedures and Implantation
Typically, HNS involves the implantation of a small stimulator device near the hypoglossal nerve. The specific surgical procedure varies depending on the individual patient's needs and anatomical characteristics. Precise placement of the stimulator is crucial for optimal stimulation efficacy and minimizing potential complications.
The surgical procedure itself involves careful planning and execution to ensure the safety and well-being of the patient. Advanced imaging techniques are often employed to guide the placement of the stimulator, providing a precise map of the hypoglossal nerve and surrounding tissues.
Patient Selection and Evaluation
Patient selection for HNS is crucial to maximize the potential benefits and minimize adverse outcomes. Thorough neurological evaluations and assessments of swallowing and speech impairments are necessary to identify suitable candidates.
Detailed patient histories, including pre-existing medical conditions and potential complications, are vital in the evaluation process. This comprehensive approach helps to identify potential risks and allows for personalized treatment plans that address individual needs.
Future Research and Development
Ongoing research is vital to further explore the potential of HNS in various neurological and medical conditions. Investigating long-term outcomes and refining stimulation protocols are crucial steps in optimizing this therapeutic approach. This includes further study into the specific mechanisms of action and the potential to personalize treatment plans for individual patient needs.
Future research could focus on developing more sophisticated and targeted stimulation techniques that further enhance the efficacy and minimize potential side effects. This will be critical in the development of new and improved treatment options for a wider range of neurological and medical challenges.