睡眠時無呼吸症の助けを見つける:リソースとサポート
May 08, 2025 / zsfcdn103/
Sleep apnea, a potentially serious sleep disorder, manifests in various ways. One unmistakable sign is loud, chronic snoring that occurs in bursts throughout the night. These snoring episodes are frequently interrupted by noticeable pauses in breathing that can last anywhere from a few seconds to over a minute. When breathing resumes, it's often accompanied by gasping or choking sounds. While not everyone who snores has sleep apnea, this symptom combined with daytime fatigue should prompt further medical evaluation.
Excessive daytime sleepiness represents another hallmark symptom. People with untreated sleep apnea often describe feeling exhausted despite spending what seems like adequate time in bed. This persistent fatigue can manifest as difficulty staying awake during routine activities like reading, watching television, or even driving. The cognitive effects are equally concerning - many patients report problems with memory, focus, and decision-making that significantly impact their professional and personal lives.
The Impact on Daily Life: Beyond the Obvious
The consequences of sleep apnea extend far beyond simple tiredness. Many sufferers experience mood disturbances including irritability, depression, and anxiety that strain relationships. Research indicates the chronic sleep fragmentation caused by apnea events may contribute to long-term cognitive decline and increased risk of dementia. Partners often report being affected as well, with many developing their own sleep issues due to the patient's loud snoring and restless sleep patterns.
Safety concerns represent another critical consideration. The impaired alertness associated with sleep apnea increases accident risk substantially - studies show those with untreated sleep apnea are 2-5 times more likely to be involved in motor vehicle accidents. Occupational hazards also increase, particularly for those operating machinery or performing precision tasks requiring sustained attention.
The Role of Snoring and Breathing Pauses
While snoring affects approximately 40% of adult men and 24% of adult women, the type associated with sleep apnea has distinct characteristics. The snoring tends to be exceptionally loud (often audible through closed doors) and follows a pattern of crescendo-decrescendo with periodic silence when breathing stops. These apneic episodes trigger micro-arousals that fragment sleep architecture, preventing restorative deep sleep stages despite adequate time in bed.
The physiological impact of these breathing pauses is significant. Oxygen saturation levels can drop dramatically during episodes, sometimes below 80%. This oxygen desaturation triggers stress responses that elevate blood pressure and heart rate. Over time, these repeated cardiovascular stressors contribute to hypertension, heart disease, and metabolic disorders.
Recognizing the Symptoms in Others
Bed partners often serve as the first line of detection for sleep apnea. Witnessing breathing pauses followed by gasping or choking sounds represents one of the most reliable indicators of potential sleep apnea. Other observable signs include restless sleep with frequent position changes, night sweats, and morning headaches. Some patients exhibit unusual sleep behaviors like sleep talking or walking that may relate to sleep fragmentation.
Daytime observations can be equally telling. Colleagues might notice excessive sleepiness during meetings, while family members may observe personality changes or decreased interest in activities. Children with sleep apnea often display hyperactivity rather than sleepiness, along with academic struggles and behavioral issues.
Seeking Professional Diagnosis and Treatment
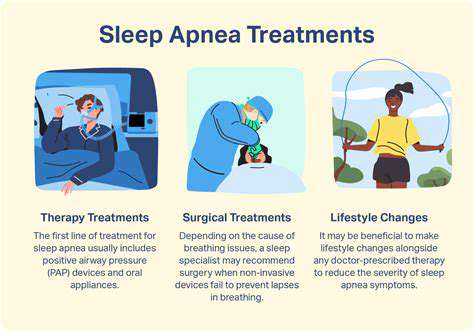
Recognizing potential symptoms should prompt medical evaluation. Modern diagnostic approaches often begin with home sleep testing, making evaluation more accessible than ever before. Comprehensive in-lab polysomnography remains the gold standard when home testing proves inconclusive or when evaluating complex cases. Treatment options have expanded significantly beyond CPAP, including oral appliances, positional therapy, and surgical innovations.
Early intervention proves critical, as research demonstrates treatment can reverse many consequences of sleep apnea. Successful management often yields rapid improvements in quality of life, cognitive function, and cardiovascular health. The key lies in matching treatment to individual needs and ensuring proper follow-up to maintain therapeutic effectiveness.
Seeking a Diagnosis and Treatment Options
Understanding the Diagnostic Process
Diagnosing sleep apnea requires a comprehensive approach that begins with detailed symptom assessment. Physicians typically use validated questionnaires like the STOP-BANG or Epworth Sleepiness Scale to quantify symptoms and risk factors. Physical examination focuses on anatomical features that may contribute to airway obstruction, such as neck circumference, jaw structure, and nasal patency.
Modern sleep studies have evolved significantly, with many patients now qualifying for convenient home sleep testing. These portable devices monitor breathing patterns, oxygen levels, heart rate, and sometimes sleep position. While not as comprehensive as in-lab studies, they provide sufficient data for diagnosing most cases of moderate to severe obstructive sleep apnea. In-lab polysomnography remains essential for complex cases, central sleep apnea, or when other sleep disorders are suspected.
Exploring Treatment Options
Treatment selection depends on multiple factors including apnea severity, anatomical considerations, and patient preferences. CPAP therapy continues to be the most effective treatment for moderate to severe obstructive sleep apnea, with modern devices offering enhanced comfort features like humidification and pressure relief. However, adherence remains a challenge for some patients, prompting development of alternative options.
Oral appliances that advance the mandible have proven effective for mild to moderate cases and CPAP-intolerant patients. These custom-fitted devices require evaluation by dental sleep specialists to ensure proper fit and efficacy. Positional therapy devices help patients who experience apnea primarily when sleeping on their back. Surgical options range from minimally invasive procedures to complex reconstructions, with success rates varying by technique and patient selection.
Emerging treatments like hypoglossal nerve stimulation offer new hope for select patients who haven't responded to traditional therapies. This implantable device activates tongue muscles during inspiration to maintain airway patency. Regardless of treatment modality, ongoing follow-up ensures therapeutic effectiveness and allows for necessary adjustments over time.
Finding Support Groups and Online Communities

Finding Local Support Groups
Local support networks provide invaluable resources for individuals navigating sleep apnea. Many hospitals and sleep centers host regular support meetings where patients can share experiences and practical tips. These gatherings often feature guest speakers including sleep physicians, respiratory therapists, and equipment specialists. The American Sleep Apnea Association maintains a directory of local chapters and support groups across the country.
Specialized groups exist for particular populations, including women with sleep apnea and parents of children with sleep disorders. These focused groups address unique challenges and provide tailored advice that general groups might overlook. Some pulmonary rehabilitation programs incorporate sleep apnea education and peer support as part of comprehensive care for patients with overlapping respiratory conditions.
Utilizing Online Support Communities
The digital landscape offers expansive support options accessible anytime. Dedicated forums like CPAPTalk and SleepApnea.org boast active communities with decades of collective experience. These platforms allow users to compare equipment, troubleshoot issues, and share success stories. Social media groups provide more immediate interaction, with many offering ask the expert sessions with sleep professionals.
Mobile apps have transformed peer support, enabling real-time troubleshooting and encouragement. Some integrate with CPAP devices to facilitate data sharing with both support communities and healthcare providers. Online platforms particularly benefit rural patients and those with mobility challenges who might otherwise lack access to in-person support.
Choosing the Right Support Group
Effective support requires finding the right fit. Consider whether you prefer structured meetings with educational components or more casual peer-led discussions. Some groups focus intensely on treatment adherence, while others emphasize emotional support and lifestyle adjustments. Many find value in trying several options before settling on their preferred community.
Online groups vary in moderation style and expertise level. Well-moderated forums with professional oversight tend to provide the most accurate information, while less regulated groups may offer more emotional support. Time zones matter for live online meetings - international groups ensure round-the-clock availability but may lack local treatment insights.
Managing Sleep Apnea: Lifestyle Changes and Long-Term Support
Improving Sleep Hygiene
Consistent sleep routines significantly benefit apnea management. Establishing fixed wake times helps regulate circadian rhythms, improving sleep quality regardless of apnea events. Creating a pre-sleep ritual signals the body to prepare for rest - this might include light stretching, meditation, or journaling. The sleep environment requires special attention: consider elevated head positioning, white noise machines, and temperature control (cooler is generally better).
Technology habits profoundly impact sleep. The blue light from screens can delay melatonin production by several hours, exacerbating sleep fragmentation. Implementing a digital curfew 1-2 hours before bed helps mitigate this effect. Some find specialized glasses that block blue light helpful when evening screen use is unavoidable.
Dietary Modifications
Nutritional choices influence both sleep quality and apnea severity. Evening meals should be light and completed several hours before bedtime to minimize reflux risk. Some patients benefit from reducing high-glycemic foods that can cause blood sugar fluctuations during sleep. Hydration timing matters - adequate daytime hydration supports mucous membrane health, while limiting fluids before bed reduces nighttime awakenings.
Emerging research suggests certain nutrients may specifically benefit sleep apnea patients. Foods rich in omega-3 fatty acids and antioxidants may help reduce inflammation contributing to airway obstruction. Some patients report improvement with magnesium-rich foods that promote muscle relaxation, though evidence remains anecdotal.
Regular Exercise
Physical activity benefits sleep apnea through multiple mechanisms. Aerobic exercise improves oxygen utilization and may reduce apnea severity independent of weight loss. Targeted exercises strengthening oropharyngeal muscles show promise in some studies. Yoga and breathing exercises can enhance respiratory control and reduce apnea-related stress responses.
Consistency proves more important than intensity when establishing an exercise routine. Even gentle activities like walking or swimming provide benefits when performed regularly. Timing matters - vigorous exercise close to bedtime may be stimulating for some, while others find it promotes sleep. Individual experimentation helps determine optimal routines.
Avoiding Certain Sleeping Positions
Positional therapy remains one of the simplest yet most effective interventions for many patients. Studies show approximately 60% of OSA patients experience significantly fewer events when sleeping on their side versus their back. Various devices help maintain side-sleeping, from specialized pillows to wearable position monitors. Some patients benefit from slight head elevation, though excessive elevation can sometimes worsen apnea.
For those struggling with positional changes, physical therapy may help. Some practitioners teach specific sleep positions that optimize airway alignment while maintaining comfort. Over time, these adjusted positions can become habitual without requiring external devices.
Seeking Professional Help
Professional guidance ensures optimal management. Sleep specialists can identify when lifestyle measures need supplementation with medical therapies. Regular follow-up allows for treatment adjustments as needs change over time. Multidisciplinary teams often provide the most comprehensive care, potentially including ENT specialists, dentists, nutritionists, and mental health professionals.
Technology now enables remote monitoring, allowing providers to track treatment efficacy between visits. Many patients benefit from periodic reassessment, as weight changes, aging, and other health developments can alter treatment needs. Establishing an ongoing relationship with a sleep care team provides the best foundation for long-term management success.