أجهزة تحفيز المسالك الهوائية العلوية: حلول مبتكرة لوقف التنفس أثناء النوم
Jun 06, 2025 / zsfcdn103/
What Are Upper Airway Stimulation Devices?
What Is Upper Airway Stimulation?
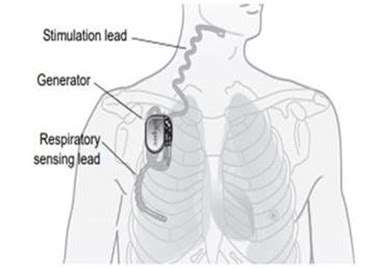
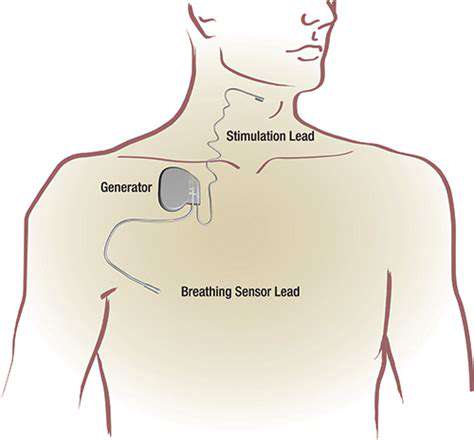
Upper airway stimulation (UAS) represents an innovative approach to managing obstructive sleep apnea (OSA). The procedure involves implanting a small device that delivers gentle nerve stimulation to maintain airway patency during sleep. Unlike traditional CPAP machines, this surgical solution offers a more permanent alternative for patients struggling with compliance.
The science behind UAS continues to evolve as researchers uncover new insights into its neurostimulatory effects. Clinical trials demonstrate particular promise for patients who've found limited success with conventional therapies. As with any medical intervention, thorough patient education remains paramount when considering this treatment pathway.
Types of Upper Airway Stimulation Devices
Modern medical technology offers several UAS device configurations, each employing distinct activation mechanisms. Some models utilize targeted electrical impulses, while others combine both electrical and mechanical stimulation principles. Selection depends on multiple clinical factors including anatomical considerations and individual response patterns.
Device longevity and adaptation to physiological changes represent critical design considerations. Ongoing clinical surveillance ensures these medical devices meet stringent safety standards throughout their operational lifespan.
Surgical Procedure and Recovery
UAS implantation typically occurs under general anesthesia using minimally invasive surgical techniques. Surgeons carefully position the device to optimize therapeutic effect while minimizing tissue disruption. The procedure's relative brevity often surprises patients expecting more extensive operations.
Postoperative protocols emphasize gradual recovery with specific activity restrictions. Multidisciplinary follow-up care significantly enhances recovery trajectories and long-term outcomes. Most patients resume normal activities within several weeks, though individual experiences may vary.
Effectiveness and Outcomes
Clinical data reveals substantial reductions in apnea-hypopnea index (AHI) scores among UAS recipients. Beyond statistical improvements, patients frequently report enhanced sleep quality and daytime functioning. Emerging longitudinal studies suggest sustained benefits may extend to cardiovascular and metabolic health markers.
Potential Benefits and Risks
The therapy's advantages include improved nocturnal oxygenation and reduced sleep fragmentation. However, surgical risks such as infection or device-related complications require careful consideration. Comprehensive preoperative evaluation helps identify optimal candidates while minimizing adverse event potential. Shared decision-making processes ensure patients understand both the therapy's promise and limitations.
How Do Upper Airway Stimulation Devices Function?
Mechanism of Action
These sophisticated devices operate through precise neurostimulation of upper airway musculature. During sleep, the implanted system detects breathing patterns and delivers timed stimulation to maintain airway patency. This dynamic response prevents pharyngeal collapse without disrupting natural sleep architecture.
Types of Stimulation
Different stimulation modalities exist, each with unique technical specifications. Some systems employ unilateral hypoglossal nerve stimulation, while others target multiple neural pathways. The selection process considers individual anatomical variations and therapeutic response profiles.
Advanced models now incorporate respiratory phase detection algorithms to optimize stimulation timing. This technological refinement enhances therapeutic precision while conserving battery life.
Factors Influencing Effectiveness
Therapy success depends on multiple variables including proper device programming and patient-specific factors. Body position during sleep, weight fluctuations, and medication use may all influence outcomes. Regular follow-up appointments allow clinicians to adjust stimulation parameters as needed.
Device efficacy typically improves during the initial adaptation period as patients and clinicians refine settings. Consistent usage remains the single most important predictor of therapeutic success.
Potential Benefits and Risks
Beyond apnea reduction, many patients experience secondary benefits like reduced nocturia and morning headaches. However, potential adverse effects including tongue discomfort or temporary swallowing changes may occur. Comprehensive informed consent processes ensure realistic patient expectations before implantation.
Considerations and Potential Drawbacks
Implantation Challenges and Risks
Surgical expertise significantly impacts procedural outcomes and complication rates. While generally safe, the implantation carries standard surgical risks plus device-specific considerations. Postoperative swelling may temporarily affect device functionality until resolution occurs.
Device-Related Issues and Malfunction
Like all implantable technologies, UAS devices require periodic evaluation for proper function. Battery depletion typically occurs after several years, necessitating replacement procedures. Modern devices incorporate sophisticated diagnostics to facilitate early problem detection.
Patient Selection and Compliance
Ideal candidates demonstrate specific polysomnographic findings and adequate anatomical characteristics. Psychological readiness for device maintenance and follow-up represents another crucial selection factor. Some patients may require temporary CPAP use during initial healing phases.
Cost and Accessibility Concerns
While insurance coverage has expanded, financial barriers persist for some patients. The total cost includes not just the device but also surgical fees and long-term follow-up care. Cost-effectiveness analyses must consider both immediate expenses and potential long-term healthcare savings.