What is CPAP? A Beginner's Guide to Sleep Therapy
May 31, 2025 / zsfcdn103/
How Does CPAP Work?
Understanding the Basics of CPAP
For those struggling with sleep apnea, Continuous Positive Airway Pressure (CPAP) therapy has become a life-changing solution. The device functions by delivering a steady stream of air that keeps the throat muscles from collapsing during sleep. This gentle pressure acts like an invisible splint, maintaining an open pathway for oxygen to flow uninterrupted. Patients often report immediate improvements in their ability to breathe normally throughout the night.
The true value of this treatment lies in its ability to restore natural breathing patterns. By eliminating the frequent awakenings caused by oxygen deprivation, CPAP allows the body to progress through all necessary sleep stages. This restoration of proper sleep architecture leads to measurable improvements in daytime alertness and cognitive function. Many users describe the difference as going from constant exhaustion to feeling truly rested for the first time in years.
The Mechanics Behind CPAP Machines
Modern CPAP units consist of three primary components working in concert. The base unit houses a quiet motor that draws in room air, filters it, and pressurizes it to the prescribed level. This treated air travels through flexible tubing to a specially designed mask that forms a secure seal around the nose or mouth. The masks now feature advanced materials that distribute pressure evenly while minimizing skin irritation.
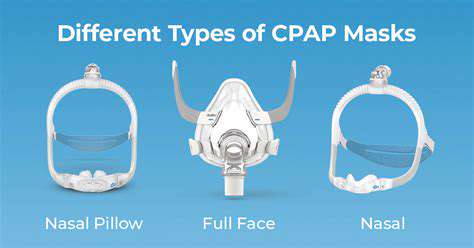
Manufacturers have made significant advancements in mask technology. Current designs accommodate various sleeping positions and facial structures, with options ranging from minimal nasal pillows to full-face coverage. The proper mask selection often determines treatment success more than any other factor. Patients should work closely with their providers to test different styles during daytime trials before committing to a particular model.
Personalizing Treatment Settings
Effective CPAP therapy requires careful calibration to each patient's physiological needs. Sleep specialists use data from overnight sleep studies to determine the minimum pressure required to prevent airway collapse. Modern machines can automatically adjust within a prescribed range, responding to changes in sleeping position or sleep stage that might affect breathing patterns.
Follow-up appointments allow clinicians to review usage data and make necessary adjustments. Many patients benefit from gradual pressure increases as they adapt to therapy. The latest devices include humidification controls and ramp features that make the initial adjustment period more comfortable. These technological improvements have significantly increased long-term compliance rates.
Complementary Lifestyle Adjustments
While CPAP provides the foundation for sleep apnea treatment, certain lifestyle modifications can enhance its effectiveness. Weight management remains crucial, as excess tissue in the neck area contributes to airway obstruction. Positional therapy, including specialized pillows or wearable devices, can help maintain optimal sleeping postures.
Regular equipment maintenance ensures consistent performance. Filters require weekly cleaning or replacement, while masks and tubing need periodic inspection for wear. Establishing a consistent bedtime routine helps synchronize the body's natural sleep-wake cycle with CPAP use. Many patients find combining these strategies creates a comprehensive approach to managing their sleep disorder.
CPAP Therapy Benefits and Side Effects
Restoring Natural Sleep Patterns
The most immediate benefit reported by CPAP users involves dramatic improvements in sleep continuity. By preventing the micro-awakenings caused by breathing interruptions, the therapy allows for complete sleep cycles. This results in deeper, more restorative sleep that leaves patients feeling refreshed in the morning. Many describe the difference as comparable to switching from a broken mattress to a premium sleep system.
Beyond simple restfulness, proper sleep architecture supports critical biological processes. Memory consolidation, hormone regulation, and cellular repair all depend on uninterrupted sleep. Patients often notice improvements in mood stability and emotional resilience as their therapy progresses, demonstrating the far-reaching impact of quality sleep.
Cardiovascular Protection
Repeated oxygen desaturation during apnea events creates significant strain on the cardiovascular system. CPAP therapy directly addresses this by maintaining constant oxygen levels throughout the night. Studies have shown consistent use can lower blood pressure comparable to some antihypertensive medications.
The reduction in sympathetic nervous system activation may explain the decreased incidence of cardiac events among compliant CPAP users. This protective effect appears particularly pronounced in patients with existing heart conditions. The therapy's ability to normalize nocturnal blood pressure patterns provides round-the-clock cardiovascular benefits.
Cognitive Enhancement
Sleep fragmentation characteristic of untreated apnea leads to measurable cognitive deficits. CPAP therapy reverses these effects by restoring proper sleep architecture. Patients report clearer thinking, improved problem-solving abilities, and better information retention within weeks of starting treatment.
Neuroimaging studies reveal structural changes in the brains of long-term apnea sufferers. Remarkably, consistent CPAP use can partially reverse these changes, demonstrating the brain's plasticity when provided with adequate oxygen during sleep. These findings underscore the importance of early diagnosis and treatment.
Metabolic Improvements
The relationship between sleep apnea and metabolic dysfunction represents an active area of research. CPAP therapy appears to improve insulin sensitivity independent of weight changes. This metabolic benefit may explain the reduced diabetes incidence observed in treated patients.
Hormonal regulation also improves with therapy. Leptin and ghrelin levels normalize, potentially reducing cravings and aiding weight management efforts. These systemic effects demonstrate how treating sleep apnea can positively influence multiple body systems simultaneously.
Addressing Treatment Challenges
Initial adaptation to CPAP therapy presents some common hurdles. Nasal congestion often responds to machine-integrated humidification systems. Mask discomfort typically resolves with proper fitting and gradual acclimation. Dry mouth may indicate mouth leaks requiring mask adjustment or chin strap use.
Persistent issues warrant consultation with sleep specialists who can adjust pressure settings or recommend alternative interfaces. The majority of side effects diminish within the first month as patients develop tolerance. Support groups and educational resources help newcomers navigate the adjustment period successfully.
Getting Started with CPAP Therapy
Recognizing Sleep Apnea Symptoms
Many individuals remain unaware they have obstructive sleep apnea, attributing daytime fatigue to aging or stress. Characteristic symptoms include witnessed breathing pauses, unrefreshing sleep, and morning headaches. Bed partners often report loud snoring interrupted by silence followed by gasping. These signs should prompt evaluation by a sleep specialist.
Risk assessment goes beyond traditional factors like obesity. Anatomical features such as a recessed chin or large tonsils can predispose individuals to airway collapse. Even fit individuals can develop apnea due to these structural factors. Comprehensive evaluation including sleep studies provides definitive diagnosis.
The Science Behind Positive Airway Pressure
CPAP technology creates a pneumatic splint in the upper airway. The continuous pressure prevents tissue collapse that occurs when throat muscles relax during sleep. This simple mechanical solution effectively treats the root cause of obstructive events without medications or surgery.
Modern devices incorporate sophisticated algorithms that respond to subtle breathing changes. Some models automatically adjust pressure throughout the night while others maintain fixed therapeutic levels. The choice between these technologies depends on individual patient characteristics and physician recommendations.
Selecting Appropriate Equipment
CPAP machine selection involves balancing features with individual needs. Basic models provide reliable therapy at lower cost, while premium units offer advanced data tracking and comfort features. Travel-friendly compact designs benefit mobile users without sacrificing performance.
Mask selection proves equally important. Nasal masks work well for nose breathers, while full-face designs accommodate mouth breathers or those with nasal obstructions. Newer hybrid designs combine the benefits of both styles. Most suppliers offer trial periods to ensure proper fit before purchase.
Establishing Effective Usage Habits
Successful CPAP therapy requires consistent nightly use. Beginners often benefit from wearing the mask during relaxing daytime activities to acclimate. Starting with shorter sleep sessions and gradually increasing duration helps build tolerance.
Proper cleaning routines maintain equipment performance and hygiene. Manufacturers provide specific guidelines for each component. Establishing these maintenance habits early prevents problems and extends equipment lifespan. Many modern machines include usage tracking to monitor compliance and effectiveness.
Integrating Therapy with Overall Health
CPAP works best as part of comprehensive health management. Weight reduction decreases pressure requirements for many patients. Alcohol avoidance in evening hours reduces airway collapsibility. Smoking cessation improves overall respiratory function.
Regular follow-up ensures ongoing treatment efficacy. Physiological changes over time may require pressure adjustments. New symptoms or recurrence of old ones should prompt reevaluation. A proactive approach to therapy management maximizes long-term benefits.