Mild Obstructive Sleep Apnea: Recognizing Symptoms and Effective Management Options
Nov 16, 2024 / zsfcdn103/
Recognizing the Symptoms of Mild Obstructive Sleep Apnea
Common Symptoms to Look For
Mild obstructive sleep apnea (OSA) often presents with a range of symptoms that can be subtle and easily overlooked. Individuals may experience excessive daytime sleepiness, which may lead to difficulties in concentration, reduced alertness, and even mood disturbances. Snoring is another hallmark symptom, particularly loud or disruptive snoring that can disturb the sleep of others. While many may dismiss snoring as a benign inconvenience, it often serves as a warning sign of underlying sleep apnea.
In addition to snoring, many patients report episodes of gasping or choking during sleep. These occurrences can awaken the sleeper, leading to fragmented sleep patterns and feelings of unrest upon waking. Other symptoms may include dry mouth or sore throat upon waking, frequent nighttime urination, and morning headaches. Recognizing these symptoms early is crucial for timely intervention and management.
The Importance of Seeking Medical Evaluation
If you or a loved one are experiencing these symptoms, it is essential to seek a professional evaluation. A healthcare provider can assess your medical history and may recommend a sleep study to confirm a diagnosis. The importance of early diagnosis cannot be overstated, as untreated mild OSA can progress into more severe forms, potentially leading to serious health complications such as cardiovascular disease, diabetes, and increased risk of accidents.
In addition to sleep studies, healthcare providers may also utilize questionnaires and assessments to better understand the severity and impact of your symptoms on daily life. With appropriate evaluation, patients can receive tailored treatment options that may include lifestyle modifications, positional therapy, or the use of oral appliances to keep the airways open during sleep.
Identifying Causes and Risk Factors
Understanding the Anatomy of Sleep Apnea
Obstructive sleep apnea (OSA) occurs when the muscles at the back of your throat relax excessively, leading to a temporary blockage of the airway. This blockage can interrupt normal sleep cycles, causing both snoring and gasping. Anatomical features such as enlarged tonsils, a thick neck, or a recessed chin can contribute to the risk of OSA. Additionally, excess fat around the neck can constrict the airway during sleep. Understanding these anatomical factors is crucial for identifying potential risk in individuals.
Another important factor is the position of the tongue, which can fall backward into the throat and obstruct the airway. This mechanical blockage plays a significant role in the severity of sleep apnea. Thus, anatomical predispositions must be considered when evaluating potential cases of OSA.
Health professionals often conduct physical examinations to assess these anatomical characteristics. Observations may include the shape of the jaw, the size of the uvula, and nasal congestion. Identifying these physical traits assists healthcare providers in predicting the likelihood of sleep apnea.
In some patients, structural anomalies in the airway can be identified, leading to a tailored approach in managing their condition. Such evaluations can help clarify if further diagnostic testing, like sleep studies, is necessary to confirm the presence of OSA.
Overall, understanding the anatomy involved in sleep apnea not only aids in diagnosis but also informs management strategies tailored to individual needs.
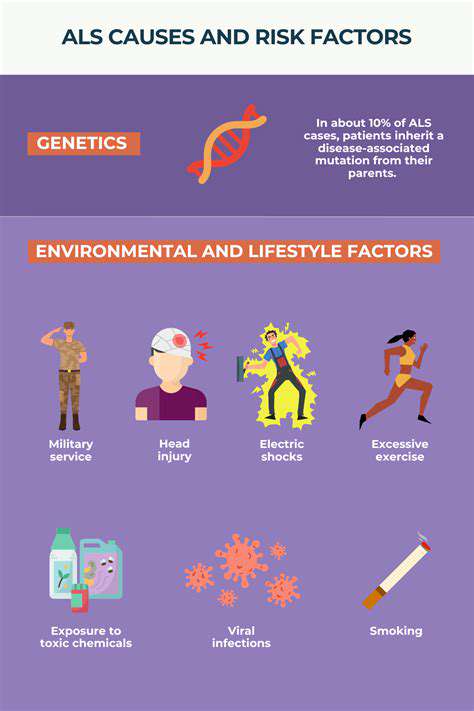
Lifestyle Factors Contributing to Sleep Apnea
Certain lifestyle choices significantly increase the risk of developing obstructive sleep apnea. Key factors include obesity, smoking, and excessive alcohol consumption. Obesity is one of the most critical risk factors, as excess weight increases the likelihood of airway obstruction during sleep.
Furthermore, smoking can inflame the upper airway, making it more susceptible to blockages. Quitting smoking may significantly reduce this inflammation, thereby lowering the risk of OSA. Alcohol consumption is another contributor, as it can relax throat muscles and further impede airflow during sleep.
Diet also plays a vital role in the management of sleep apnea. A diet high in carbohydrates can contribute to weight gain, exacerbating the condition. Conversely, adopting a balanced diet that fosters weight loss can mitigate the severity of sleep apnea symptoms.
Regular physical activity is essential not only for weight management but also for enhancing overall sleep quality. Engaging in exercise can help reduce the severity and frequency of sleep apnea episodes and promote healthier sleep patterns.
In summary, making informed lifestyle choices can significantly impact the development and management of sleep apnea. A commitment to a healthier lifestyle is a proactive step towards reducing risk factors.
Genetic and Familial Influences on Sleep Apnea
Genetics play a notable role in the development of obstructive sleep apnea. Studies show that individuals with a family history of sleep apnea are at a higher risk of developing the condition themselves. Hereditary traits may include predispositions to obesity or anatomical features contributing to airway obstruction.
Research has also suggested that certain genetic variations might influence the breathing patterns and responsiveness of the airway muscles during sleep. This can lead to episodes of apnea or hypopnea, affecting overall sleep quality.
In families where sleep apnea is common, it can be helpful for members to undergo periodic screenings, particularly if they exhibit symptoms like loud snoring or excessive daytime sleepiness. Early identification can lead to prompt intervention and management.
Additionally, understanding familial patterns can inform healthcare providers about potential risks in other family members, prompting preventive measures. Raising awareness around genetic risk factors may encourage individuals to be vigilant about symptoms, leading to early diagnosis and treatment.
Overall, recognizing the genetic contributions to obstructive sleep apnea highlights the importance of family history in assessing risk and guiding treatment options.
Age and Its Effect on Sleep Patterns
As individuals age, they often experience changes in sleep architecture, which can increase the likelihood of developing obstructive sleep apnea. Older adults tend to have a more significant amount of relaxed muscle tone during sleep, leading to higher rates of airway obstruction.
Furthermore, age-related conditions such as hypertension or diabetes can exacerbate the severity of sleep apnea symptoms. Older adults may also experience changes in body composition, including increased fat retention in the neck area, further raising the risk of airway obstruction during sleep.
Additionally, the ability to identify and report sleep disturbances often declines with age, which can lead to underdiagnosed or untreated conditions. Healthcare providers need to be vigilant in assessing symptoms of sleep apnea in older patients, as they may be more prone to complications.
When managed properly, older adults can experience significant improvements in sleep quality and overall health. Screening for sleep apnea in geriatric populations can enhance quality of life and mitigate potential health risks associated with untreated sleep disorders.
In conclusion, age is a significant factor in the incidence and management of obstructive sleep apnea, highlighting the need for tailored approaches for older individuals.
Medical Conditions That Increase the Risk of Sleep Apnea
Various medical conditions can contribute to the development and severity of obstructive sleep apnea. Common comorbidities include hypertension, type 2 diabetes, and cardiovascular diseases. These conditions often exacerbate the symptoms of sleep apnea and can create a vicious cycle of health complications.
Individuals with hypothyroidism may also be at increased risk, as this condition can lead to weight gain and obesity, both of which are significant risk factors for OSA. Additionally, neurological disorders such as Parkinson's disease can affect the brain's ability to regulate breathing during sleep.
Another critical factor is the presence of gastroesophageal reflux disease (GERD), which can worsen sleep apnea symptoms by irritating the airways. This irritation may prompt individuals to adopt sleep positions that further complicate their breathing.
Those with chronic respiratory diseases, like asthma or COPD, are also more likely to experience obstructive sleep apnea due to compromised airflow. Understanding the link between these medical conditions and sleep apnea is essential for effective management and treatment.
In summary, addressing underlying health conditions is crucial for individuals suffering from obstructive sleep apnea. A comprehensive approach that considers all concurrent health issues will lead to better overall outcomes.
Effective Management Strategies
Understanding Mild Obstructive Sleep Apnea
Mild obstructive sleep apnea (OSA) is a common sleep disorder characterized by intermittent pauses in breathing during sleep. These interruptions can lead to inadequate sleep quality and can cause feelings of fatigue during the day. Recognizing the symptoms is crucial for early intervention and effective management. Many people may experience mild OSA without realizing it, making awareness and education essential.
Common symptoms of mild OSA include snoring, gasping for air during sleep, and excessive daytime sleepiness. If left untreated, the condition could potentially progress, leading to more severe health issues. Some individuals may also experience difficulty concentrating, mood changes, or memory problems as a result of fragmented sleep.
Mild OSA can be influenced by several risk factors, such as obesity, age, gender, and anatomical features like the size of the neck or airway. Understanding these factors can aid individuals in recognizing their susceptibility to the disorder. Additionally, lifestyle choices such as alcohol consumption and smoking can exacerbate symptoms.
Diagnosis often involves a sleep study, which may be conducted at a sleep clinic or through home-monitoring devices. A healthcare professional can help interpret the results and recommend appropriate treatment options. Early detection and management prevent potential complications associated with moderate to severe sleep apnea.
Awareness of the signs and symptoms of mild obstructive sleep apnea is the first step towards seeking help. Educating oneself and others can lead to timely diagnosis and management, improving overall sleep health.
Lifestyle Changes for Effective Management
Implementing lifestyle changes can significantly improve the management of mild obstructive sleep apnea. One of the most beneficial adjustments includes maintaining a healthy weight, as excess weight can contribute to airway obstruction. Regular exercise not only supports weight loss but also enhances overall respiratory function.
Avoiding alcohol and sedatives is crucial since these substances can relax the throat muscles, increasing the likelihood of airway blockage during sleep. Establishing a consistent sleep routine can also help, as going to bed and waking up at the same time each day promotes better sleep quality.
Sleep position plays an important role in managing sleep apnea symptoms. Sleeping on the back may worsen breathing difficulties, while sleeping on the side can help keep the airway open. Utilizing pillows or specialized devices to promote side sleeping can be beneficial.
Regular follow-up with a healthcare provider ensures that management strategies are working effectively. Adjustments to lifestyle factors or treatment options may be necessary based on symptoms and overall health condition. Continuous monitoring can lead to improvements and sustained management of symptoms.
Committing to these lifestyle changes may take time, but the benefits for sleep quality and overall health are substantial. A proactive approach can result in lasting improvements and a better quality of life for those with mild obstructive sleep apnea.
Medical and Therapeutic Options
In addition to lifestyle modifications, various medical options are available for managing mild obstructive sleep apnea. Continuous positive airway pressure (CPAP) therapy is a common treatment that keeps the airway open during sleep by delivering a constant flow of air. Although often associated with moderate to severe cases, mild patients may also benefit from a less invasive approach.
Dental appliances, or oral appliances, can be an effective treatment option as well, especially for individuals who are unable or unwilling to use CPAP. These custom-fitted devices help reposition the jaw to keep the airway open. Consulting a dental specialist experienced in sleep apnea treatment is essential for choosing the right device.
For those with identifiable anatomical issues contributing to their OSA, surgical options may be considered. Surgical interventions can range from uvulopalatopharyngoplasty (UPPP) to more advanced procedures aimed at correcting structural abnormalities. It is vital to discuss the risks and benefits of surgery with a qualified healthcare provider.
Behavioral therapies, including cognitive behavioral therapy for insomnia (CBT-I), can also be effective in managing sleep-related issues associated with mild OSA. These therapies target the psychological aspects of sleep disorders, fostering better sleep habits and reducing anxiety around sleep.
Ultimately, the management of mild obstructive sleep apnea should be individualized, considering the patient's specific symptoms and preferences. Collaborative care among healthcare providers, sleep specialists, and patients is essential for achieving optimal outcomes.