How COPD Affects CPAP Usage: Key Considerations
May 08, 2025 / zsfcdn103/

Mask Selection and Comfort in COPD Patients
Mask Selection Considerations for COPD Patients
Choosing the right mask is absolutely critical for COPD patients relying on CPAP therapy. Several factors come into play, including the patient's unique facial structure, whether they experience nasal congestion, and any coexisting conditions like sinusitis or rhinitis. A mask that doesn't fit properly can cause more than just discomfort—it may lead to skin problems and even make breathing more difficult, potentially undermining the entire treatment. The market offers various CPAP mask styles—nasal masks, full face masks, and nasal pillows—each with distinct advantages. The ideal choice varies from patient to patient based on their specific requirements.
Impact of Nasal Congestion on Mask Comfort
For COPD patients, nasal congestion isn't just an annoyance—it can seriously interfere with CPAP treatment. The continuous air pressure from the machine might actually worsen nasal blockage, creating a vicious cycle of discomfort and poor compliance. Those with persistent nasal issues often struggle with nasal masks, as the device can aggravate already sensitive nasal passages. In such cases, exploring different mask designs becomes necessary to maintain treatment effectiveness.
Importance of Proper Mask Fit and Pressure
The success of CPAP therapy hinges on achieving the perfect mask fit. An ill-fitting mask creates painful pressure points that may develop into skin sores, making treatment unbearable. Taking time to properly adjust the straps and cushions can make all the difference between abandoning therapy and successful long-term use. Equally important are the pressure settings, which should be carefully calibrated by a medical professional to balance comfort with therapeutic effectiveness.
Addressing Skin Irritation and Breakouts
Extended CPAP use, particularly for COPD patients, often leads to skin problems. The constant contact and pressure can cause irritation and even pressure ulcers, directly impacting treatment adherence. Simple solutions like choosing hypoallergenic materials, applying protective moisturizers, and ensuring proper fit can prevent these issues. Regular skin checks should become part of the patient's routine to catch problems early.
CPAP Mask Alternatives for COPD Patients
When traditional CPAP masks prove too uncomfortable, alternatives exist. Nasal pillows or full face masks might offer better tolerance. The decision depends on multiple factors including individual sensitivity, facial structure, and the severity of nasal obstruction. Working closely with healthcare providers to test different options ensures patients find the most suitable solution.
Patient Education and Compliance
Successful CPAP treatment requires thorough patient education. Understanding why the therapy matters, how to achieve proper fit, and what side effects might occur dramatically improves compliance. Healthcare teams should provide comprehensive materials and ongoing support to help patients overcome challenges and stick with their treatment plan.
Long-Term Mask Management and Maintenance
Maintaining CPAP equipment properly is crucial for both effectiveness and hygiene. Regular cleaning prevents dangerous bacterial or mold growth that could cause infections. Following manufacturer guidelines for care and promptly replacing worn components ensures the mask continues to function as intended while remaining comfortable for the user.
Managing COPD Exacerbations and CPAP Therapy
Understanding COPD Exacerbations
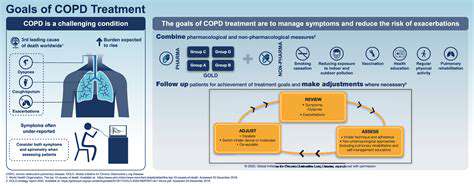
COPD flare-ups represent sudden symptom worsening that demands immediate medical intervention. These episodes range from mild discomfort to life-threatening emergencies. Spotting early warning signs and understanding triggers forms the foundation of effective management and complication prevention. Various factors—from infections to environmental pollutants or medication changes—can spark exacerbations, requiring personalized treatment approaches.
During flare-ups, patients typically experience intensified shortness of breath, increased coughing, and changes in phlegm production and color. These symptoms dramatically affect daily functioning, making ordinary activities challenging. Early recognition allows for prompt treatment, potentially preventing progression to more severe stages.
Managing Triggers and Preventing Exacerbations
Environmental irritants significantly contribute to COPD flare-ups. Air pollution, smoke (including secondhand), and other airborne irritants can precipitate symptom worsening. Proactively minimizing exposure to known triggers represents a crucial strategy for maintaining respiratory stability. This includes improving indoor air quality and avoiding polluted environments whenever possible.
Respiratory infections like influenza or pneumonia frequently trigger exacerbations. Vaccination serves as a critical preventive measure. Regular healthcare visits for immunizations and check-ups form the cornerstone of preventative care for COPD patients. Combined with healthy lifestyle choices—proper nutrition and appropriate exercise—these measures support lung health and reduce exacerbation risks.
Medication changes, whether new prescriptions or dosage adjustments, sometimes contribute to symptom worsening. Regular medication reviews with healthcare providers help identify potential issues. Proper inhaler technique and understanding of respiratory medications ensure their optimal effectiveness in preventing flare-ups.
Effective Treatment Strategies During Exacerbations
Prompt treatment during exacerbations is essential. Bronchodilators help relax constricted airways, while supplemental oxygen may become necessary to maintain adequate blood oxygen levels. In severe cases, hospitalization ensures proper monitoring and comprehensive care through a team approach involving various specialists.
CPAP Therapy and Oxygen Therapy Integration

CPAP Therapy
CPAP (Continuous Positive Airway Pressure) therapy remains the gold standard for obstructive sleep apnea treatment. The machine delivers constant air pressure through a sleep mask, preventing airway collapse characteristic of OSA. When used consistently, CPAP dramatically improves sleep quality and reduces OSA symptoms while lowering risks of serious complications like hypertension and cardiovascular disease.
Treatment effectiveness varies based on OSA severity, patient compliance, and equipment quality. Close collaboration with healthcare providers ensures proper CPAP settings and addresses any usage difficulties. Regular equipment checks and adjustments maintain optimal therapy effectiveness.
Oxygen Therapy
For patients struggling with oxygen absorption, supplemental oxygen therapy provides vital support. This treatment benefits those with COPD, cystic fibrosis, and other lung conditions. By reducing respiratory strain, oxygen therapy enhances comfort and overall health outcomes while improving gas exchange efficiency in compromised lungs.
Therapy parameters are carefully tailored to individual needs under medical supervision. Careful monitoring of blood oxygen levels and appropriate flow rate adjustments ensure safe, effective treatment while preventing potential complications.
Differences and Considerations
While both therapies address breathing issues, they serve distinct purposes. CPAP maintains open airways during sleep, while oxygen therapy directly boosts blood oxygen levels. These treatments aren't interchangeable—some patients require one, the other, or both simultaneously depending on their specific condition.
Medical professionals must evaluate each case individually to determine the appropriate therapeutic approach. Self-treatment with either modality without proper guidance poses significant risks and should be strictly avoided. The decision between CPAP, oxygen therapy, or their combination requires thorough clinical assessment and personalized care planning.