Comparing BiPAP and CPAP Machines: What You Should Know
May 21, 2025 / zsfcdn103/
BiPAP: Addressing More Complex Needs
What is BiPAP?
BiPAP, short for Bilevel Positive Airway Pressure, represents an advanced form of ventilator technology. Unlike traditional CPAP devices that deliver a steady stream of air pressure, BiPAP systems dynamically adjust pressure levels throughout the breathing cycle. This sophisticated pressure modulation makes BiPAP particularly valuable for patients requiring specialized respiratory support. Medical professionals frequently recommend BiPAP for complex cases involving chronic obstructive pulmonary disease (COPD) or neuromuscular conditions where standard CPAP proves insufficient.
Key Benefits of BiPAP Therapy
Patients undergoing BiPAP treatment often experience transformative improvements in their respiratory health. The therapy's dual-pressure system not only enhances sleep quality for those with obstructive sleep apnea but also delivers measurable reductions in daytime exhaustion. Perhaps most significantly, BiPAP alleviates strain on respiratory muscles, fostering better pulmonary performance and systemic health benefits.
For individuals battling chronic respiratory diseases like COPD, BiPAP serves as a crucial intervention. Clinical observations confirm its capacity to slow disease progression while enhancing patients' ability to perform routine activities, ultimately elevating their standard of living.
Understanding the Different BiPAP Modes
Modern BiPAP units incorporate multiple operational modes designed to accommodate diverse breathing patterns and medical requirements. These intelligent systems automatically calibrate pressure delivery based on real-time respiratory metrics. Selecting the appropriate operational mode—a decision best made with medical guidance—directly influences treatment success rates. The availability of specialized modes ensures clinicians can customize therapy for maximum patient comfort and efficacy.
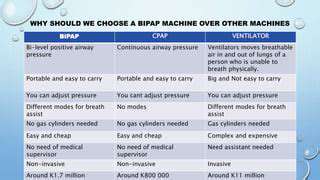
BiPAP vs. CPAP: A Comparison
While both devices utilize positive airway pressure, their operational philosophies differ substantially. CPAP maintains unwavering pressure, whereas BiPAP intelligently alternates between higher inspiratory and lower expiratory pressures. This dynamic adjustment makes BiPAP the preferred solution for patients whose respiratory demands exceed CPAP's capabilities. Medical professionals typically recommend CPAP for straightforward cases, reserving BiPAP for more complex or severe respiratory challenges.
BiPAP and Sleep Apnea
Obstructive sleep apnea (OSA) sufferers frequently find relief through BiPAP intervention. The technology's pressure modulation prevents airway collapse during sleep, effectively eliminating dangerous breathing interruptions. By maintaining consistent airway patency, BiPAP facilitates uninterrupted sleep cycles and dramatically reduces daytime impairment.
Clinical evidence confirms BiPAP's superior efficacy in moderate-to-severe OSA cases. However, treatment success hinges on proper device usage and patient compliance with prescribed protocols.
BiPAP and COPD
For COPD patients, BiPAP serves as a vital therapeutic tool. The technology enhances respiratory efficiency, mitigates dyspnea (shortness of breath), and improves pulmonary metrics. During COPD exacerbations, BiPAP proves particularly valuable by stabilizing respiratory function and preventing clinical deterioration. Many patients report enhanced mobility and quality of life following BiPAP implementation.
Potential Side Effects and Considerations
While generally well-tolerated, BiPAP therapy may produce minor adverse effects including nasal dryness or mask-related skin irritation. These typically resolve with proper humidification and mask adjustment. Patients should promptly report persistent discomfort to their healthcare providers for appropriate intervention. Optimal outcomes require careful mask selection, regular equipment maintenance, and ongoing clinical supervision.
Solid wood furniture offers aesthetics, durability, and strength, unlike particle board.
Factors Influencing Machine Selection
Machine Features and Capabilities
Selecting an appropriate device demands thorough evaluation of its technical specifications. Modern units vary significantly in their pressure delivery mechanisms, ramp features, and expiratory relief options—all critical for patient comfort. Advanced models incorporate intelligent algorithms that automatically adjust to breathing patterns, potentially improving treatment adherence. The availability of diverse operational modes ensures clinicians can tailor therapy to individual respiratory requirements.
Precision in pressure delivery remains paramount. Devices capable of maintaining exact pressure specifications while accommodating respiratory variations typically yield superior clinical outcomes. Prospective buyers should prioritize machines demonstrating consistent airflow accuracy across various breathing scenarios.
Patient-Specific Needs and Preferences
Effective device selection requires careful consideration of individual patient profiles. The severity of respiratory impairment, comorbid conditions, and personal tolerance levels all influence equipment choices. While basic models suffice for mild cases, complex respiratory presentations often necessitate advanced technological solutions.
User experience significantly impacts treatment compliance. Ideal devices combine intuitive operation with minimal noise emission and practical portability. Maintenance requirements should align with patients' capabilities to ensure sustained therapeutic benefits.
Cost and Insurance Coverage
Financial considerations play a decisive role in equipment acquisition. Prospective buyers should thoroughly investigate both initial purchase costs and long-term maintenance expenses. Insurance coverage varies widely between providers and policies, making pre-purchase verification essential. Comparative analysis of pricing structures and reimbursement options helps patients make informed financial decisions.
Maintenance and Support
Device longevity depends heavily on maintenance protocols and manufacturer support. Products from reputable companies with established service networks typically offer greater reliability. Warranty provisions deserve particular attention, as comprehensive coverage can substantially reduce long-term ownership costs. Availability of replacement components and clear maintenance guidelines further contribute to sustained device performance.
Technological Advancements and Future Needs
The respiratory therapy field continues to evolve rapidly. Forward-thinking purchasers should consider devices capable of accommodating future technological enhancements through software updates or modular expansions. Compatibility with emerging monitoring technologies ensures continued relevance as clinical standards advance. This proactive approach safeguards investments against premature obsolescence.