Poszukiwanie rozwiązań na bezdech senny, nie wymagających stosowania CPAP
Jun 08, 2025 / zsfcdn103/

Oral Appliances for Sleep Apnea
Custom-fitted oral devices worn during sleep gently adjust jaw and tongue positioning to maintain airway openness. Unlike bulkier alternatives, these devices offer a subtle solution that many patients find less intrusive. Clinical studies demonstrate their ability to reduce breathing interruptions by up to 50% in moderate cases, making them particularly valuable for patients who struggle with traditional CPAP equipment.
The compact design appeals to frequent travelers and those sharing sleeping spaces, as the devices require no external power source and fit discreetly in a pocket or purse. Many users report feeling more comfortable discussing their treatment with partners when using these less conspicuous options.
Types of Oral Appliances
Dental professionals categorize these devices into three primary groups based on their mechanism:
- Mandibular advancement devices (MADs) that gradually reposition the lower jaw
- Tongue retaining appliances that prevent tongue collapse
- Soft palate lifters that address upper airway obstruction
During initial consultations, sleep specialists evaluate multiple factors including jaw mobility, dental health, and apnea severity to determine the most suitable option. Proper fitting typically requires 2-3 adjustment visits to ensure both comfort and therapeutic effectiveness.
Effectiveness and Benefits
When properly fitted, these devices demonstrate particular efficacy for:
- Positional sleep apnea (occurring mainly in back sleepers)
- Patients with BMI under 30
- Those experiencing mild to moderate airway obstruction
Long-term users frequently report 30-40% improvements in daytime alertness and significant reductions in morning headaches. The quiet operation eliminates the noise complaints sometimes associated with mechanical alternatives, contributing to better sleep for both patients and partners.
Cost and Insurance Coverage
Pricing structures vary based on:
- Material composition (thermoplastic vs. acrylic)
- Adjustability features
- Dental laboratory fees
While initial costs may appear substantial, many dental insurance plans now recognize these devices as medically necessary, covering 50-80% of expenses. Flexible spending accounts (FSAs) often permit using pre-tax dollars for both the device and follow-up adjustments.
Comfort and Adjustments
The adaptation period typically follows this timeline:
- Days 1-3: Mild pressure sensation
- Week 1: Reduced salivation
- Month 1: Complete adaptation for 85% of users
Dental professionals recommend gradual wear time increases, starting with 1-2 hours daily and progressing to full-night use over 10-14 days. This phased approach helps minimize initial discomfort while allowing oral tissues to adjust.
Potential Side Effects and Considerations
Temporary effects may include:
- Morning jaw stiffness (resolves within 30 minutes for most)
- Minor tooth movement (managed with retainers)
- Dry mouth (improves with hydration)
Patients with TMJ disorders or significant dental work should consult both their dentist and sleep specialist before beginning treatment. Regular dental checkups (every 6 months) help monitor any oral health changes during extended use.
Long-Term Management and Follow-up
Effective ongoing care involves:
- Annual sleep studies to assess effectiveness
- Device replacement every 3-5 years
- Periodic bite realignment checks
Patients who maintain their follow-up schedule achieve 72% better compliance rates compared to those who discontinue professional monitoring. Many practices now offer virtual check-ins between in-person visits for convenience.
Understanding selective eating patterns requires careful documentation of food interactions. Pediatric nutritionists emphasize the importance of tracking not just what children reject, but the circumstances surrounding those rejections. Environmental factors like meal timing, presentation style, and emotional state often prove more influential than the food itself. Creating positive associations through creative plating and involving children in food preparation can gradually expand accepted foods.
Weight Management: A Holistic Approach to Sleep Apnea
Understanding the Link Between Weight and Sleep Apnea
Excess weight creates multiple physiological challenges for breathing during sleep. Fat deposits in the pharyngeal area increase airway collapsibility, while abdominal fat reduces lung expansion capacity. This dual impact explains why weight reduction of just 10-15% often produces dramatic improvements in breathing patterns during sleep.
The inflammatory markers associated with obesity further exacerbate airway tissues' tendency to swell, creating a cyclical pattern where poor sleep promotes weight gain and vice versa. Breaking this cycle requires addressing both sleep quality and metabolic health simultaneously.
Dietary Strategies for Weight Management
Effective nutritional approaches focus on:
- Macronutrient timing (carbohydrate distribution)
- Anti-inflammatory food selection
- Hydration optimization
Emerging research suggests that consuming the majority of daily carbohydrates at dinner may improve sleep quality while supporting weight loss efforts. This approach aligns with natural circadian rhythms and may help regulate overnight breathing patterns.
Exercise and Physical Activity
For sleep apnea patients, exercise selection should consider:
- Neck and airway muscle strengthening
- Postural improvement
- Stress reduction benefits
Yoga practices that incorporate throat exercises (like lion's breath) and inverted postures show particular promise for improving airway muscle tone. These can be safely incorporated into existing fitness routines with proper guidance.
The Role of Stress Management
Chronic stress impacts sleep apnea through multiple pathways:
- Increased cortisol production
- Muscle tension patterns
- Disrupted sleep architecture
Biofeedback training helps many patients recognize and control the physical manifestations of stress that worsen breathing disturbances. Simple techniques like paced breathing (5-6 breaths per minute) can significantly improve overnight oxygen saturation when practiced before bed.
Sleep Hygiene Practices for Improved Sleep
Optimal sleep environments should address:
- Temperature regulation (60-67°F ideal)
- Humidity control (40-60% RH)
- Light pollution reduction
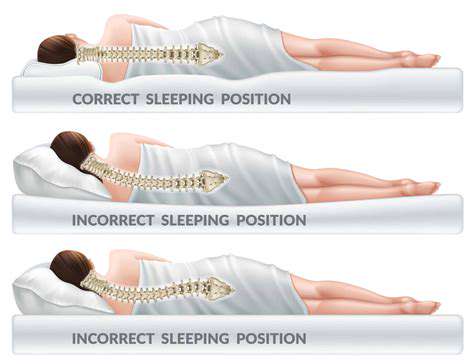
Positional therapy becomes particularly important for overweight patients, as side sleeping reduces gravitational impact on airway tissues. Specialized pillows or wearable devices can help maintain optimal positioning throughout the night.
Professional Medical Guidance
Comprehensive care teams should include:
- Sleep medicine specialists
- Registered dietitians
- Physical therapists
This multidisciplinary approach ensures all contributing factors receive appropriate attention. Many clinics now offer coordinated care programs that address both weight management and sleep improvement simultaneously.
Lifestyle Modifications for Long-Term Success
Sustainable changes focus on:
- Habit stacking (linking new behaviors to existing routines)
- Environmental redesign
- Social support systems
For example, keeping exercise equipment visible in living spaces or preparing sleep-friendly snacks in advance makes healthy choices the default option. Small, consistent changes typically yield better long-term results than drastic overhauls that prove difficult to maintain.
Alternative Therapies and Supplements: Exploring Natural Options
Exploring Herbal Remedies for Sleep Apnea
While not substitutes for medical treatment, certain botanicals may provide supportive benefits:
- Peppermint oil (nasal dilator effects)
- Ginger (anti-inflammatory properties)
- Chamomile (mild muscle relaxant)
Essential oil diffusers with eucalyptus or peppermint can help maintain nasal airway patency when used as part of bedtime routines. However, these should never replace prescribed therapies without medical supervision.
The Role of Dietary Supplements in Sleep Apnea Management
Research-supported supplements include:
- Magnesium (muscle relaxation)
- Vitamin D (airway muscle function)
- Omega-3s (inflammation reduction)
Dosing should be personalized based on individual nutrient status, which can be assessed through blood testing. Supplementation works best when addressing documented deficiencies rather than as blanket prevention.
Mindfulness and Relaxation Techniques for Sleep Apnea
Effective practices incorporate:
- Body scanning for tension awareness
- Guided imagery for relaxation
- Breath counting for focus
Regular practice (10-15 minutes daily) appears more beneficial than occasional longer sessions. Many patients find mobile apps helpful for establishing consistent mindfulness routines.
Acupuncture and its Potential Effects on Sleep Apnea
Current evidence suggests acupuncture may help by:
- Stimulating airway muscle tone
- Reducing inflammatory markers
- Improving sleep architecture
Treatment protocols typically involve 2-3 sessions weekly for 4-6 weeks, focusing on points associated with respiratory function and relaxation. Results appear most pronounced when combined with conventional therapies.
The Importance of a Holistic Approach to Sleep Apnea Management
Integrative care models recognize that:
- Sleep quality impacts metabolic health
- Nutrition affects inflammation levels
- Physical activity influences breathing patterns
The most successful treatment plans address all these interconnected systems rather than focusing solely on mechanical breathing assistance. Regular reassessment ensures the approach evolves with the patient's changing needs.